AARP Update
FIXING THE CAREGIVING SYSTEM
Policymakers at all levels are coming to the same conclusion: Family caregivers need greater support. New programs and laws are beginning to provide it

In May 2022, the AARP Bulletin published a comprehensive report on the challenging state of family caregiving and the key areas that required more attention to ease the massive burden on those who must provide regular aid to aging loved ones. The situation remains dire: By 2030, one-fifth of the U.S. population will be at least 65, meaning that more people than ever will need daily assistance of some sort.
But something noteworthy has happened since our report of 18 months ago: progress. There are signs of increasing awareness of the need to support caregivers, and a variety of state, local and federal government initiatives are being implemented.
“Almost everyone is either going to be a caregiver or will need care at some point in their life,” says Nancy LeaMond, AARP chief advocacy and engagement officer. “I think so many more decision-makers are experiencing that personally and are seeing it affect many of their constituents.”
A 2023 AARP report titled “Valuing the Invaluable” finds family caregivers provide an average of 18 hours of unpaid care per week, a commitment often overlooked by policymakers, until now. “Caregiving really crosses every demographic. It’s every race, every religion, it’s every income bracket,” LeaMond says. “We’re hearing across the political spectrum, across the states, ‘How do we work on these issues? What are some of the options for how we can move forward?’ And I think that’s particularly exciting.”
Here is an update on six areas where solid steps are being taken to help caregivers.
A NATIONAL STRATEGY
For the first time, the federal government has a plan. One year ago, the Department of Health and Human Services (HHS) released the National Strategy to Support Family Caregivers, the nation’s first official blueprint to address this need. It is intended to mobilize support of unpaid caregivers in five main areas:
▶︎ Increasing awareness of their issues and outreach to those in need.
▶︎ Building partnerships and engagement with family caregivers.
▶︎ Strengthening services and support available to caregivers.
▶︎ Ensuring their financial and workplace security.
▶︎ Expanding data, research and evidence-based practices.
The national strategy, which comes with initial funding of $20 million to be doled out in grants from the Administration for Community Living (a division of HHS created in 2012), outlines nearly 350 federal actions and more than 150 community, state-based and private-sector actions to help bolster caregiver health, well-being and financial security, with a time frame to implement federal actions within three years. After the release of the national strategy, President Joe Biden issued an executive order detailing more than 50 actions his administration will take.
“This is a tremendous time for family caregiving,” says Jason Resendez, president and CEO of the National Alliance for Caregiving. One small piece of the national strategy details broader definitions of the terms “family,” “caregiving” and “family caregivers,” an acknowledgment of the many different kinds of people doing this unpaid work, including friends and neighbors. “It’s certainly not sufficient, but the awareness of caregiving and caregivers is at levels that we haven’t seen before,” Resendez says.
MORE PAID LEAVE
The pandemic rocked the caregiver world at every age and income level; suddenly, tens of millions of Americans needed prolonged care, often at home, due to COVID-19.
More states are putting into place legislation to expand paid work leave for family caregivers. Maine, for example, adopted a paid family and medical leave program that will go into effect in 2025. Employers and employees will split a 1 percent payroll tax to fund the program, allowing workers to take up to 12 weeks of paid leave each year to care for a sick family member. State Sen. Mattie Daughtry, an author of the bill, says she is “thrilled” that it got passed into law after 10 years of trying.
NEW PAID FAMILY LEAVE LAWS
▶︎ MAINE: Up to 12
weeks/year (starts 2025)
▶︎ MINNESOTA: Up to 12
weeks/year (starts 2026)
▶︎ ILLINOIS: Up to 40
hours/year (starts 2024)
Another expansive bill was signed into law this year in Minnesota, allowing workers to take up to 12 weeks for family leave and up to 12 weeks for one’s own serious medical condition, up to a maximum of 20 weeks annually, beginning Jan. 1, 2026. To fund the program, payroll premiums will be split between employers and employees. Workers can use the paid leave to care for someone not related by blood or marriage, such as a significant other, neighbor or friend.
Toni Kay Mangskau, 58, of Rochester, Minnesota, knows how much relief this will bring. She cared for her ailing parents before they died, and at the same time was caring for her brother and her two children, all of whom had pressing medical needs. “It’s that phrase,” she says, “the sandwich generation.”
NEW FAMILY CAREGIVING COMPENSATION PROGRAMS:
▶︎ OKLAHOMA: Tax credit, up to $3,000 per year (in effect in 2024)
▶︎ UTAH: Direct payments for caregiving work, through Medicaid
Mangskau, a single mother, never knew when she’d get a call about one of them being in an emergency room or otherwise needing her help, she says. She often had to take sick or vacation leave or go without pay. She recalls that once, when her children were young, she couldn’t pay the rent. When she decided to get help at an agency, a male social worker told her she needed to sell her car and “you need to get remarried.”
Mangskau has spent nine years advocating for paid caregiving leave. “Right now, knowing that that bill passed, I can breathe more. Other people are not going to struggle,” she says. “I wanted to be able to say I stood up and shared my story and that’s what made the difference.”
Illinois also passed a law allowing for broader use of paid time off for any reason. The law provides employees with up to 40 hours of paid leave during a 12-month period, starting Jan. 1.
REAL FINANCIAL SUPPORT
In 2021, the economic value of family caregivers’ unpaid contributions was about $600 billion. They often also incur caregiving-related expenses. While some states have instituted small forms of tax relief, Oklahoma is being heralded as the first state in the nation to adopt an expansive caregiver tax credit with its Caring for Caregivers Act, which becomes law on Jan. 1. The legislation will allow a tax credit up to 50 percent of eligible caregiver costs, capped at $2,000 per year for most participants and $3,000 per year for those caring for veterans or people with a dementia-related diagnosis. Eligible expenses range from big-ticket items, such as installing a ramp, to less costly expenses, such as a walker. Hiring a home care aide, respite care, adult day care, personal care attendants and health care equipment are other eligible expenditures.
In Utah, a bill was passed this year allowing for more caregivers to be compensated for their work—actual weekly pay going into their pockets. During the COVID-19 pandemic, when paid caregivers were not able to come into homes, the state expanded a Medicaid program for spouses to include parents and legal guardians to be paid for the work and services they provided. The state Legislature voted to make it a permanent fixture. This means that spouses and guardians of an individual using Medicaid waiver services (allowing for care in a home instead of a long-term facility) can be paid for up to 40 hours per week to provide extraordinary direct care to their loved one.
“Over 1,000 families are now significantly benefiting from caregiver compensation in Utah,” says Lisa Thornton, a lawyer and longtime advocate. Thornton struggled to find stable outside caregiver help for her severely disabled daughter and found that her own care was the most successful. Thornton began receiving $593 a week for her role as caregiver. The bill is especially significant, says Alan Ormsby, AARP Utah state director, because it “creates a culture in Utah of recognizing the work being done by family caregivers that could allow this program to be expanded to someday creating similar programs for caregivers outside of Medicaid.”
PAYMENT FOR TRAINING
Family members are often drawn suddenly and without guidance into a caregiving role, leaving them on their own to figure out how to perform a range of tasks they’ve never done before.
A new proposal from the Centers for Medicare & Medicaid Services (CMS) would help with that, authorizing Medicare payments to health care professionals to train family caregivers in a range of activities, from managing medications to helping with daily living.
“Caregivers are reluctant to ask for assistance until they reach a point of crisis.”
—Nevada caregiving report
“At the highest level, I’m really excited about it,” says Tara English, CEO of Givers Health, a health care training organization based in the San Francisco Bay Area. “They are for the first time ever providing reimbursement for a person who is not a patient.”
CMS Director Meena Seshamani says that family members fill a key role on a care team that includes medical professionals and social workers.
“We see caregivers as a very important part of our overall vision for the Medicare program,” she said at an AARP-sponsored Politico virtual event in December. “How do we think about the people we’re caring for in a broader sense? Where we can provide training and education … that is key.”
GREATER OUTREACH
Most new caregivers eagerly want information and support. But navigating a maze of agencies and organizations is challenging. Federal and state programs are of little use if caregivers don’t know about them.
On the federal level, President Biden’s national strategy includes this goal: “Optimize existing family caregiver support efforts by reducing redundancy, improving information sharing and infusing best practices systemwide.”
“This is a long game,” explains Megan O’Reilly, vice president in AARP’s government affairs office. “And the executive order set out the directive to the federal government to start working on this stuff.”
In Louisiana, a new fund has been established to improve access to in-home care services.
On the state level, Nevada is working to gain a greater understanding of caregivers’ needs. The Nevada Lifespan Respite Care Coalition, an advisory board established under the Nevada Aging and Disability Services Division, spent more than a year talking to family caregivers, service providers, state agencies and recipients before publishing its first State Plan for the Support of Family Caregivers. The report offers 18 recommendations for state and community partners to consider when designing programs for family caregivers in three areas: collaboration, outreach and funding. One example: Respite services need to “be available for purchase through a sliding scale on income eligibility, so that all caregivers can purchase the service.” Another recommendation, centered on outreach, notes that “caregivers are reluctant to ask for assistance until they reach a point of crisis.”
The state Legislature authorized a study to assess the capabilities, needs and quality of life. “This bill allows lawmakers to assess the needs of family caregivers and report back to the full Legislature in 2025 with bills to enhance existing programs,” says Erin Neff, an associate state director in AARP’s Nevada office.
CLOSING THE INEQUITY GAP
One of the most challenging caregiving issues is dealing with income, racial and other disparities. Take the common example of an older person on Medicaid who is coping with a serious chronic disease. They wish to stay in their home, but if they are not eligible or not able to get home care, they may wind up in a Medicaid-funded nursing home. Medicaid does grant waivers that mean it will pay for in-home care, but they have been hard to get.
Louisiana has seen major progress, though: It gained 500 additional slots for Home and Community Based Services (HCBS) waivers for Medicaid recipients this year, allowing for services to be administered at home. “We’re chipping away at the waitlist, which is pretty lengthy,” says Andrew Muhl, AARP director of advocacy for Louisiana. “But if I wanted to go to a nursing home tomorrow, there would be a spot for me.”
He’s particularly optimistic about a “huge win” that went into effect on July 1, creating a trust fund that will place 12 percent of “any excess revenue” in a given budget year from the state into an account that could be used for HCBS needs. “It’s not a silver-bullet solution,” he says, but “it’s a sizable step in the right direction.”
A similar fund was set up in Louisiana for children with disabilities in 2007. That program has no waitlist now.
Another important action aimed at helping those who have not had access to care comes from Biden’s executive order. The recently announced Medicare Dementia Care Model aims to improve the quality of life for people living with dementia by helping them remain in their homes while reducing strain on unpaid caregivers. CMS will test a new payment for participants who deliver supportive services to people with dementia. This will include care coordination, access to a help line and a care navigator who can help find services.
Although this will affect a broad range of people, the announcement from CMS specifically noted that Black, Hispanic and Asian Americans, Native Hawaiian and Pacific Islander populations have been “particularly disadvantaged” in receiving dementia care. This Guiding an Improved Dementia Experience (GUIDE) model—running for eight years starting in July 2024—will provide new resources and greater access to specialty dementia care in “underserved populations and communities.”
Ann Oldenburg, a former USA Today reporter, is assistant director of Georgetown University’s journalism program. She has a master’s degree from Georgetown’s Aging & Health program.
FACES OF CAREGIVING
These people are working to improve caregiving—and have been caregivers themselves.
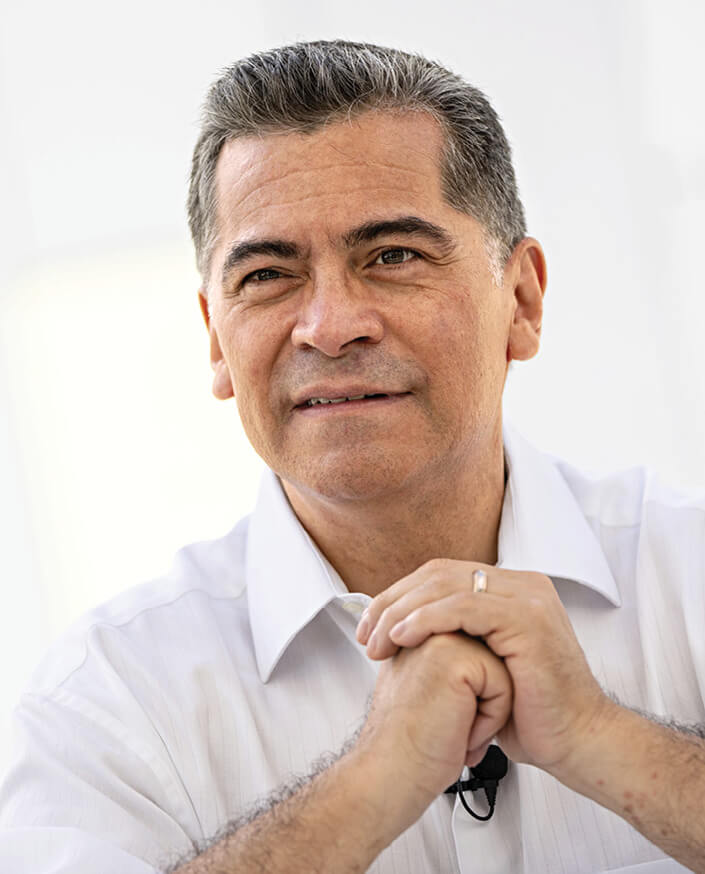
Xavier Becerra, 65 Health and Human Services secretary
CAREGIVER FOR: His parents
“In 2017, I decided to make sure we got a house so we could have my parents move in with us. For those last few years that my dad was alive, we became his caregivers, especially during his last six months to one year during hospice care. My wife and I are very fortunate that we are able to afford it, because most families can’t. In fact, many families do it even though they can’t afford it because there is no choice.
So [we’re] making sure Medicare adapts to provide families the opportunity to have the one you love stay with you instead of sending them off to a nursing home or some long-term care facility. You will find that now you will possibly qualify for federal support, financial support to care for your family members because you’re essentially doing what someone else would do if you had to send them off to a facility. That becomes a big game changer for families that want to provide the care but don’t believe they have the financial capacity to offer it.
If I were to tally up the amount of money that my wife's family saved the taxpayers [caring for her parents] and how much my family saved the taxpayers by not sending our parents to long-term care facilities, it’s got to be hundreds of thousands of dollars. It’s not just about beauty and dignity, it is just a smart thing to do.”
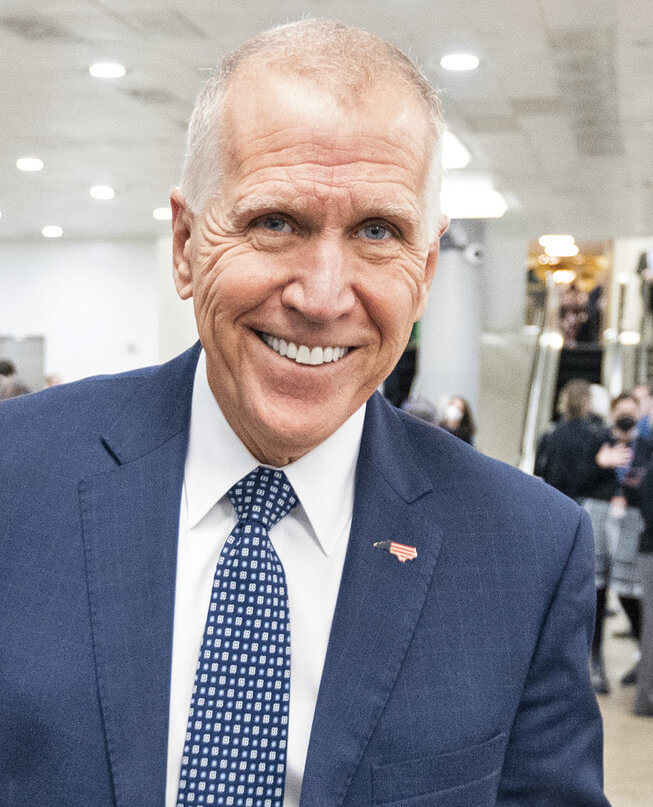
Sen. Thom Tillis, 63 (R-N.C.)
Tillis is the top Republican on the Senate Finance Subcommittee on Social Security, Pensions and Family Policy.
WAS CAREGIVER FOR: His grandmother, who developed Alzheimer’s in the mid-’90s.
“My grandmother lived independently in a sort of family setting. Her daughters lived on either side of her. She started having the classic problems; she wrecked her car coming out of the driveway. So they had to limit what she could do. I got involved explaining to my mom and aunts that she really needed full-time care. There was a really nice facility 7 miles from where she lived. We got her over there. It demonstrated to me that there are limits to what a loved one can do to provide care without dramatically changing their life.”

Sen. Maggie Hassan, 65 (D-N.H.)
Hassan is an original cosponsor of the Better Care Better Jobs bill that would enhance funding for home-and community-based care.
IS CAREGIVER FOR: Her son, Ben, 35, who has cerebral palsy and lives with her and her husband, Tom.
“We have a team who has helped us, but we have more often than not been the night shift for caregiving. And if a nurse calls in sick or a respite worker can’t come, Tom or I or our daughter are going to be the people who take care of Ben [in the daytime]. It does make you realize how tenuous the situation can be. It’s one of the things that’s really helped me focus on policy that would stabilize the system. There is growing recognition that this is not just good for people and respects people’s independence, but it is essential as we work to stabilize our health care system and grow our economy.”

Rep. Judy Chu, 70 (D-Calif.)
Chu cosponsored the Better Care Better Jobs Act to beef up home-and community-based care.
WAS CAREGIVER FOR: Her father, who had respiratory ailments
“We did hire caretakers in shifts 24 hours a day, and that was to allow him to remain in the home, which is what his greatest desire was. He was in such capable hands during the hardest months of his life. Our caregivers play such an important role in so many family lives. But caregivers are not adequately paid. We also need to have expanded paid family and medical leave options so that those who have to stay home to care for a sick loved one are more easily able to do so. We need to have 12 weeks paid family leave and to be able to take care of parents. Everybody has the potential to face the same issue. This affects so many millions of families all across America. That’s why we have to make this investment to improve our system.”

Karen Appert, 57
Coleads the Caregiver and Patient Engagement work group of the North Carolina Serious Illness Coalition
WAS CAREGIVER FOR: Her mother, who had multiple sclerosis and dementia
“In my advocacy role, one of the biggest challenges I see is that there isn’t a lot of help for people who are middle-income. And so you wind up doing a lot of it on your own. You basically learn by doing. We help our volunteers use their lived experience to advocate for better support in North Carolina. For instance, there’s the Lifespan Respite Program. In our state, a caregiver could only get up to $500 toward respite, which if you’re dealing with someone with 24/7 needs, $500 isn’t going to go very far. So it would be advocating for increased funding.”

Carrie Shaw, 35
CEO of Embodied Labs The company produces a virtual reality platform that allows people to experience what life is like with Alzheimer’s and other conditions.
WAS CAREGIVER FOR: Her mother, who had Alzheimer’s
“I became a primary caregiver for my mom when I was 23. It was just so hard for me to understand what her world was like. Why was she saying, ‘I want to go home?’ Why was she trying to pack a bag and leave the house? Now, with my work at Embodied Labs, they [caregiver and loved one] can connect with each other and problem-solve some of the most challenging things that come with caregiving.”

MaryClare Feighan, 69
Founded a caregivers’ support group in Eugene, Oregon.
IS CAREGIVER FOR: Her husband, who has spinal stenosis, fibromyalgia, osteoarthritis and deteriorating vision
“Isolation is a huge problem with caregivers. Every one of us express gratitude on a regular basis for having this group. Each of us have learned new ways to approach difficult conversations in caregiving. There’s such a great need. It would be really lovely if our government could appreciate the amount of time and energy that caregivers put in because we’re keeping our spouses alive and out of more expensive medical care.”
–Interviews by Tamara Lytle, Julie Goldenberg and Jim Lenahan
Companies Start to Step Up
Businesses recognize that caregiving benefits are needed

More than 60 percent of caregivers work full-or part-time jobs, making the average of 18 hours they spend per week on caregiving particularly challenging. Yet if they need time off to tend to the needs of a loved one, their choices typically are few: Take vacation days, sick days or unpaid leave. That is starting to change: A rising number of employers offer caregiving benefits as a way to attract and retain quality employees.
“My employer allows me to work remotely and have flexible hours, to care for my soon-to-be 97-year-old mother, who lives alone in Birmingham,” says Girtha Perkins, 66, a senior regulatory analyst based in Indianapolis. Her mother has severe arthritis in her spine and knees and is under pain management. “I think that flexibility I have is why I am still working and haven’t retired.”
According to the Society for Human Resource Management, caregiving-friendly companies are offering benefits that include more work-from-home opportunities and the ability to transition to part-time work or work-sharing, in which two employees split what would be a full-time position.
Some go beyond that. “We have some employer clients who are starting to get creative in the way they try to support employee caregivers,” says Claudia Fine, chief professional officer at eFamilyCare, a telemedicine company. Examples include connecting family caregivers with in-home respite care and providing care advice and referrals to community resources.
Fannie Mae, a mortgage financing company, instituted a program that offers up to 12 weeks of paid employee leave to care for a seriously ill family member; it also provides eldercare consultants.
CHANGING EXPECTATIONS
The COVID-19 pandemic sparked a revolution in workplace expectations, and some companies have discovered that employees who are family caregivers suffer from mental health challenges that can impact their job performance.
“The demands on employees to balance work and family commitments are more intense than ever before,” says Denise King, vice president of global benefits and payroll for Medtronic, a health technology company. Her company offers caregivers mental health support and paid time off, up to six weeks every 24 months.
Medtronic also started providing support through Wellthy, a third-party care concierge. “Employees are matched with a dedicated care coordinator, who can help manage care in any capacity, big or small,” King says. That can include assistance hiring in-home care, understanding Medicare benefits, home modifications, meal delivery, transportation and end-of-life support.
Advocates encourage more companies to treat family caregivers with the same respect as they give to parents of young children.
“We talk a lot about cradle to grave,” says Karen Kavanaugh, chief of strategic initiatives at the Rosalynn Carter Institute for Caregivers, “but right now, it is mostly the cradle.”