In the News
MEDICARE TO COVER WIDESPREAD USE OF ALZHEIMER’S DRUG

For the first time, the Food and Drug Administration (FDA) has approved for general use a drug found to slow the progress of Alzheimer’s disease, opening the door for people over 65 in the early stages of the disease to have most of their expenses covered by Medicare.
The FDA has OK’d widespread use of the drug lecanemab, sold as Leqembi. Previously, the drug had been approved only for people participating in clinical trials. “This is a big deal,” says Ronald Petersen, director of the Mayo Clinic Alzheimer’s Disease Research Center. “We’ve been waiting for this kind of breakthrough for many, many years.”
The Centers for Medicare & Medicaid Services promised to pay a large share of the cost of taking the drug once the FDA issued its broad approval. Leqembi has a projected annual cost of $26,500. That means patients with traditional Medicare or a typical Medicare Advantage plan, each of which covers 80 percent of Part B drug costs, could still pay more than $5,000 out of pocket annually to use the drug, says an estimate from KFF, a nonprofit health care research group.
The medication significantly reduced the amount of fibrous deposits known as amyloids in patients’ brains, and slowed the loss of thinking and memory skills in people with early to mild Alzheimer’s by 27 percent over an 18-month period.
“Today’s action is the first verification that a drug targeting the underlying disease process of Alzheimer’s disease has shown clinical benefit in this devastating disease,” said Teresa Buracchio, acting director of the Office of Neuroscience at the FDA, when the approval was issued in July.
The drug is not for people already deeply affected by Alzheimer’s, experts say.
The medication is given by intravenous infusion every two weeks at a hospital or medical center. Side effects range from flu-like symptoms to swelling and bleeding in the brain.
Social Security COLA Increase Smaller in 2024
SOCIAL SECURITY BENEFICIARIES, who got big boosts in their cost-of-living adjustments (COLAs) the past two years as inflation soared, will likely see a more modest increase of 3 percent in their monthly checks next year.
That projected increase, based on recently released government economic data, would boost the average Social Security retirement benefit by about $55 a month in 2024.
Emerson Sprick, of the Bipartisan Policy Center, estimates the 2024 COLA, slated to be announced in October, will land at about 3 percent. This year’s COLA was 8.7 percent, and last year’s was 5.9 percent. Through the 2010s, the COLA averaged 1.5 percent.
Social Security COLAs are tied to the Consumer Price Index for Urban Wage Earners and Clerical Workers (CPI-W), a measure of monthly price change for a selection of food, energy and other things.
A rise in the Medicare Part B premium in 2024 would offset a portion of the COLA increase for Social Security recipients who have premiums deducted from their benefit payments. In their 2023 annual report, Medicare’s trustees estimated the Part B premium would be $174.80 a month next year, up $9.90 from the current rate.
‘TRIPLE VAX’ COMING THIS FALL
MANY OLDER ADULTS will be encouraged to get not one or two, but three vaccines as weather turns cooler. The newest addition deals with a growing respiratory threat.
Nearly half of all adults got the flu shot last season. And older people are being urged to get a COVID-19 booster, which is getting an update in time for autumn.
But new this year for adults 60-plus is a vaccine for RSV, or respiratory syncytial virus, which hospitalizes as many as 160,000 older adults each year and kills up to 10,000.
“We have learned over the last 20 years that [RSV] probably causes as much illness as influenza,” says William Schaffner, of the National Foundation for Infectious Diseases.
RSV hit the U.S. especially hard last fall, and the Food and Drug Administration approved two versions of an RSV vaccine in May. The shots are expected to be available in the fall. Though the COVID-19 and flu vaccines can be taken together, experts advise getting the RSV shot separately.
Overdose Deaths Rise Sharply for Older Americans
FATAL DRUG OVERDOSES among older Americans, which have been rising for two decades, spiked even higher in recent years, according to a study published in JAMA Psychiatry.
Overdose deaths among people 65 and over from all causes, including suicides and accidents, rose 50 percent, from 4,469 in 2019 to 6,702 in 2021.
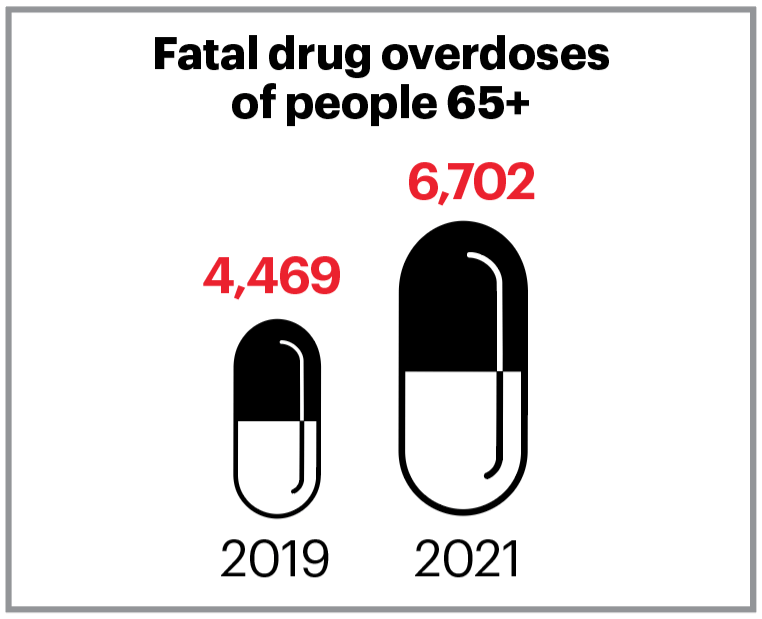
Though these are still a small percentage of the roughly 100,000 overdose deaths recorded in the U.S. each year, the study shows the continuation of an alarming trend. The rate of deaths from overdose quadrupled among older adults from 2002 to 2021, from 3 per 100,000 people to 12 per 100,000.
Several factors are to blame, the study says. One major cause: The opioid crisis that began in the late 1990s saw many Americans become addicted to drugs prescribed for pain relief. Some of them have turned to dangerous street drugs laced with fentanyl—an opiate 50 times more potent than heroin.
“No group is untouched,” says Chelsea Shover, a coauthor of the study. “We’re seeing sharp increases across the board, including in older adults who previously had low overdose mortality rates.”
PICKLED

THE PICKLEBALL CRAZE is bringing fun to workouts for older Americans. It’s also driving a boom in hip replacements, knee operations and other joint procedures, say financial analysts at UBS Group AG. The investment bank estimates injuries to “picklers” will cost $250 million to $500 million in 2023.