feature story
By Sari Harrar
illustration by sean mccabe
BREAKTHROUGHS IN
CHRONIC PAIN
‘Whole Health’ Relief for Pain Management

Heath Haug says his life is less limited by pain.
HEATH HAUG SERVED for 22 years in the Army, Marine Corps and National Guard, followed by two decades as a cop. “I beat my body up,” he says. “My back, feet, my knee. It takes a toll.”
But now Haug, 54, of Christiansburg, Virginia, has found relief through the Salem Veterans Affairs Health Care System’s (VAHCS) innovative Prevail Center for Chronic Pain. The program gives veterans basic coping strategies through an online or face-to-face “pain school,” after which they meet for an hour with a caregiving team—made up of a psychologist, a pharmacist, a dietitian, a physical therapist and a physician specializing in pain—that creates a personalized, six-month treatment plan focused on healthy eating, exercise, spirituality and reducing stress.
Haug has lost 12 pounds by eating more produce and less packaged food. He’ll soon start cognitive behavioral therapy for insomnia and has received injections to ease arthritis in his spine. Soon he hopes to get back to hiking with his wife. “The pain’s going to be there,” he says. “I’m learning ways to minimize it to lead a normal life.”
Haug is among Prevail’s first group of 280 participants, who have reported that their pain is no longer controlling their life, says clinical psychologist Rena Courtney, director and creator of Prevail.
“We start by asking, ‘If you were in less pain, what would you be doing more of?’ We get answers like ‘I’d be playing with the grandkids,’ or ‘I’d be hunting or fishing,’ ” Courtney says. “We tell them that’s how we’re going to know if we’re successful—if you’re doing more of that in six months.”
Chronic pain affects approximately 37.8 million midlife and older Americans, and nearly a third have high-impact pain that makes daily life difficult. In 2019, the Department of Veterans Affairs called on the National Academies of Sciences, Engineering and Medicine to study the potential of the whole health care model that Courtney and others at the VA are using to address chronic pain.
Prevail is offered only at the Salem VAHCS; Courtney suggests civilians with chronic pain look for pain programs affiliated with medical schools or ask their doctor for referrals for help with diet, exercise, stress, sleep and mental health. The VA’s free, online Personal Health Inventory (va.gov/wholehealth/phi.asp) can help you get started.
What matters is taking a holistic approach to pain management, says Courtney—one that treats the biological and emotional aspects.
“When I ask, ‘What happens to your pain when you’re stressed,’ every single person says it gets worse,” she says. “If pain were just biological, that wouldn’t matter.”
MORE CHRONIC PAIN BREAKTHROUGHS
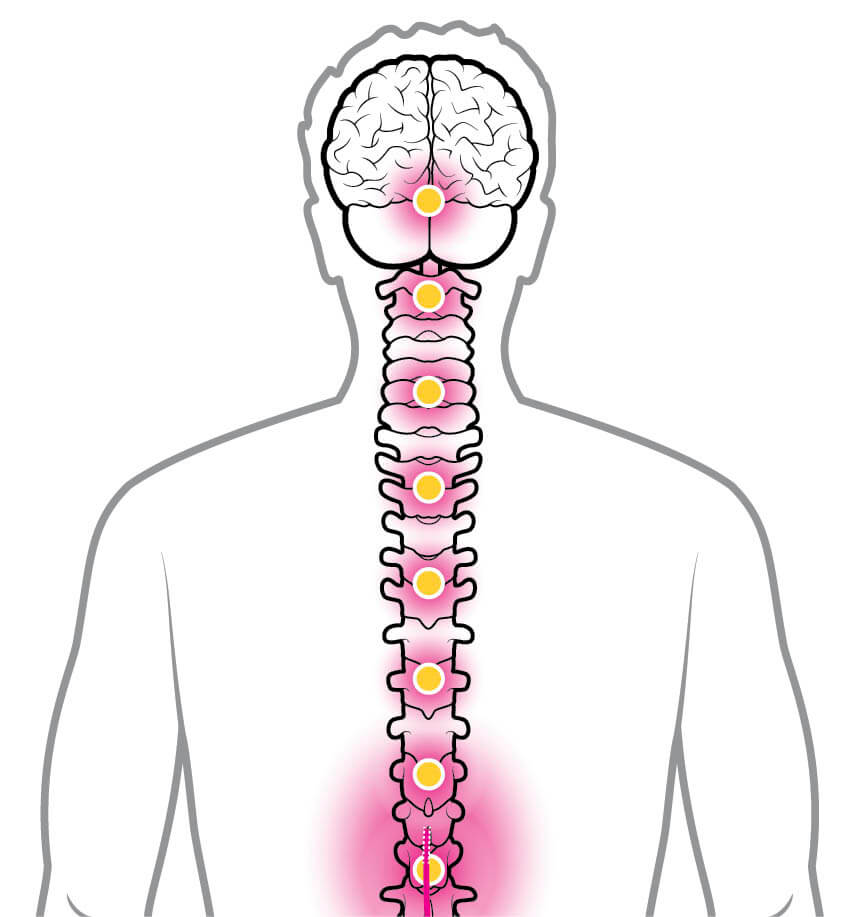
Drug-Free Help for Diabetic Nerve Pain
Early in 2023, the FDA approved use of the Eterna, Proclaim Plus and Proclaim XR Spinal Cord Stimulation (SCS) Systems to relieve lower-extremity pain caused by diabetic peripheral neuropathy (DPN). The devices send mild electrical signals to the spinal cord, reducing pain by an average of 53 percent in studies.

Virtual Reality for Back Pain
A virtual reality program called RelieVRx, by AppliedVR, successfully reduced back pain by half for 46 percent of users who followed the program daily for eight weeks. Users of the prescription-only system put on a VR headset to learn cognitive behavioral skills for pain management such as deep relaxation and breathing exercises. Sessions last two to 16 minutes. The program is currently available in some health systems and through the Department of Veterans Affairs.
ON THE HORIZON
NEW USES FOR NALTREXONE
► Once prescribed for alcohol and opioid overuse, the drug naltrexone is getting new attention for its potential to ease pain from Crohn’s disease, fibromyalgia, rheumatoid arthritis and more. University of Kansas Medical Center scientists recently reviewed naltrexone, concluding that it shows promise, but more research is needed.
BREAKTHROUGHS IN
WOMEN’S HEALTH
3D Ultrasound for Better Mammograms

A new no-compression scan for dense breasts
LORI MILLER USED to feel relieved when her mammogram results arrived in the mail. “They’re always normal,” she says. But in recent years, there’s been a puzzling postscript. “The letter explains that I have ‘dense breasts,’ which makes it harder to find cancer on a regular mammogram,” she says. That made her “normal” results feel less than fully reassuring.
This year, Miller, 58, a retired industrial engineer from Pontiac, Michigan, tried something new. First, she had a conventional mammogram. Then she walked down the hall at the Barbara Ann Karmanos Cancer Institute in Detroit for a three-dimensional whole-breast ultrasound screening called SoftVue, recently granted premarket approval by the Food and Drug Administration as an add-on cancer check for dense breasts. Called a 3D whole-breast ultrasound tomography system, the new technology sends sound waves to create a 360-degree image of the breast that offers a more comprehensive look at the tissue—without compressing or sending radiation completely through the breast—showing tissue changes in detail. The results? Normal. “It was nice knowing the results would provide increased cancer detection,” Miller says.
Cancer risk is up to four times higher in dense breasts, possibly because dense tissue has more cells that can become abnormal, and women with dense breasts may have higher levels of estrogen, which can increase the risk of cancer. Conventional mammograms may miss up to 40 to 60 percent of cancers in dense breasts, says Rachel Brem, M.D., director of breast imaging and intervention at George Washington University in Washington, D.C.

Lori Miller finds relief in her tests.
Clinical data has shown that scans with SoftVue, plus a conventional mammogram, found 20 percent more cancers than mammograms alone—and were better at weeding out false positives, says Brem. “This is a new kind of ultrasound,” she adds. “It gives us more information about tissue character.” A 2020 study found that the system measured breast tumor changes early in chemotherapy—potentially useful for seeing if treatment is working or not. The system can also detect the stiffness of breast tissue and differentiate between malignant and benign masses, another study found.
About 40 percent of women in their 50s and 30 percent of women 60 and older have dense breasts, but just 38 states require breast-imaging centers to inform women of the issue. (A new FDA rule requires all U.S. mammogram facilities to notify patients about their breast density starting in September 2024.) The American Cancer Society suggests women with dense breasts discuss screening strategies with their doctors; options include 3D X-ray mammography, other types of ultrasound tests or an MRI, often along with a standard mammogram.
“Women with dense breasts really need additional screening,” Brem says.
MORE WOMEN’S HEALTH BREAKTHROUGHS

New Hot Flash Drug
The FDA in May approved a nonhormonal treatment for menopausal hot flashes and night sweats. Veozah (fezolinetant) blocks a receptor on brain cells that plays a role in temperature regulation. The drug, intended for moderate to severe hot flashes, significantly reduced the number and severity of episodes in clinical trials.
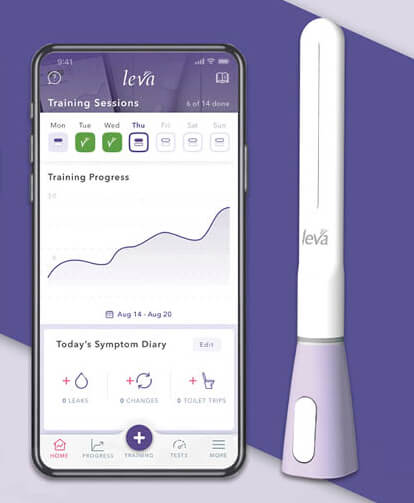
High-Tech Help for Incontinence
In a study, participants using a prescription-only pelvic-floor training device called leva Pelvic Health System, which delivers feedback to a smartphone app, reported significantly greater improvement in incontinence versus those exercising on their own.
ON THE HORIZON
BONE HEALTH INSIGHTS FROM ASTRONAUTS
► A growing stack of studies is delving into bone loss in astronauts on spaceflights and aboard the International Space Station, with results that could mean stronger skeletons and better fraction prevention on Earth. And insights into how bone strength and density recover from space travel may yield new targets for osteoporosis-fighting treatments in the future for women and men.
BREAKTHROUGHS IN
CARDIOVASCULAR DISEASE
Device Busts Lung Clots Three Ways

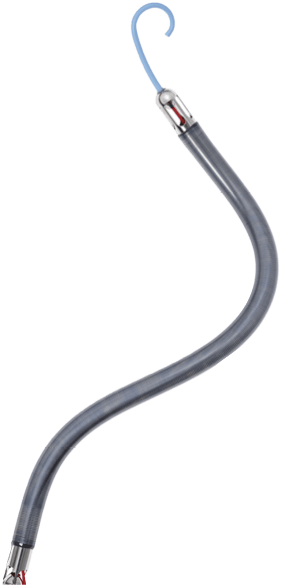
This catheter unclogs arteries while delivering clot-dissolving drugs.
TIM CRONIN, 82, grew short of breath as he raked leaves in his Warrington, Pennsylvania, yard one Monday in November 2019. By Friday, he could barely breathe. Large blood clots—pulmonary embolisms—had blocked blood flow in his lungs, boosting pressure on the right side of his heart and restricting delivery of blood to the rest of his body. Fortunately, his doctors had a new clot-busting treatment.
Cronin became an early recipient of the Bashir Endovascular Catheter, a device that’s threaded through the blood vessels to the lungs, then opens into an expandable infusion basket in the clot, creating multiple channels to allow for blood flow, while the catheter’s arms spray a clot-dissolving drug directly into the blood clot. “People clapped and yelled hooray when the first catheter was put in place,” recalls Cronin, who was awake during the procedure. He needed two, to open blockages in both lungs. He spent the first night at Doylestown Health with the device in place, returning home a few days later, after the clots had diminished. Several months after that, he rode his bike about 125 miles during a weeklong beach vacation.
Tim Cronin is back to living an active lifestyle.
Pulmonary embolisms (PEs) are the third-leading cause of cardiovascular death in the U.S. behind heart attack and stroke, hospitalizing 350,000 people per year and causing more than 100,000 deaths. The clots usually form in deep veins in the legs and travel upward to the lungs. But the Bashir and Bashir S-B Endovascular catheters, cleared by the FDA in 2023 for pulmonary embolisms, are part of a growing number of treatments for medium-risk PEs, which affect up to 65 percent of people with the condition. PEs need aggressive care to prevent heart and lung damage.
While our bodies produce natural clot busters of their own, when blood can’t flow, those natural compounds can’t reach the obstruction.
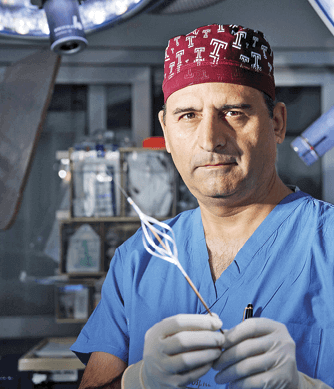
Device inventor Riyaz Bashir, M.D.
“I wanted to design a device that could create multiple channels for blood to flow into the clot, bringing in the body’s own clot-dissolving chemicals,” says device inventor Riyaz Bashir, M.D., director of Vascular and Endovascular Medicine at Temple University in Philadelphia. “That can mean life and death for a patient. All of a sudden blood starts oxygenating, and the patient starts feeling better.”
The device’s catheter has six mini infusion catheters, each with laser-drilled holes that expand into the obstruction and then saturate it with a clot-busting drug. That, plus the assist from natural clot busters in blood, “reduces the dose of medicine, which reduces risk for bleeding,” Bashir says. The treatment takes about five hours.
Four years after his lung clots, Cronin takes medication to reduce his risk for future problems. “My heart seems fine,” he says. “And I’m back to raking leaves.”
MORE CARDIOVASCULAR BREAKTHROUGHS


Women’s Heart Centers
A study found that women with a common, but often-overlooked, type of heart disease caused by narrow or spasming arteries had major improvements in chest pain, anxiety, blood pressure and cholesterol levels when they were treated at a women’s heart center.
A Little Pump Lets the Heart Rest and Recover
A tiny, temporary pump is now available to give the heart time to get up to speed after right-side heart failure. Implanted through a groin incision, the FDA-approved Impella RP System helps the heart move blood to the lungs to receive oxygen.
ON THE HORIZON
AN EXPERIMENTAL ‘TATTOO’ TO TRACK HEART HEALTH
► University of Texas at Austin scientists are studying a lightweight grid that spreads across the chest like a tattoo, monitoring electrical and acoustical signals from the heart without requiring the wearer to stay at a medical center.
BREAKTHROUGHS IN
DIABETES
A Continuous Glucose Monitoring Revolution
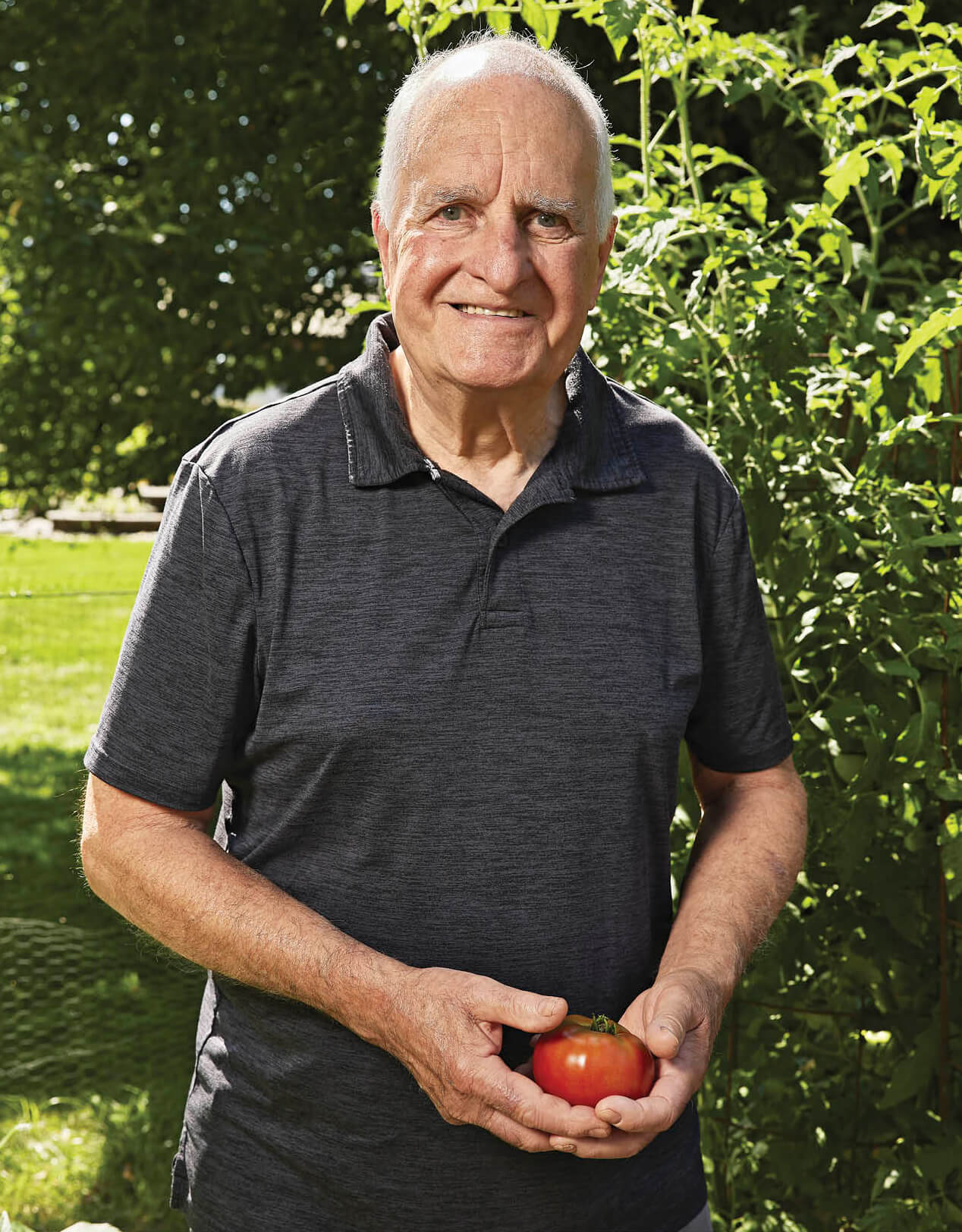
Andy Pincus controls his blood sugar with a CGM.
DIAGNOSED WITH type 2 diabetes in 2004, Andy Pincus has made some radical changes. He’s lost 52 pounds, walks more than 15,000 steps a day and eats a more plant-based diet.
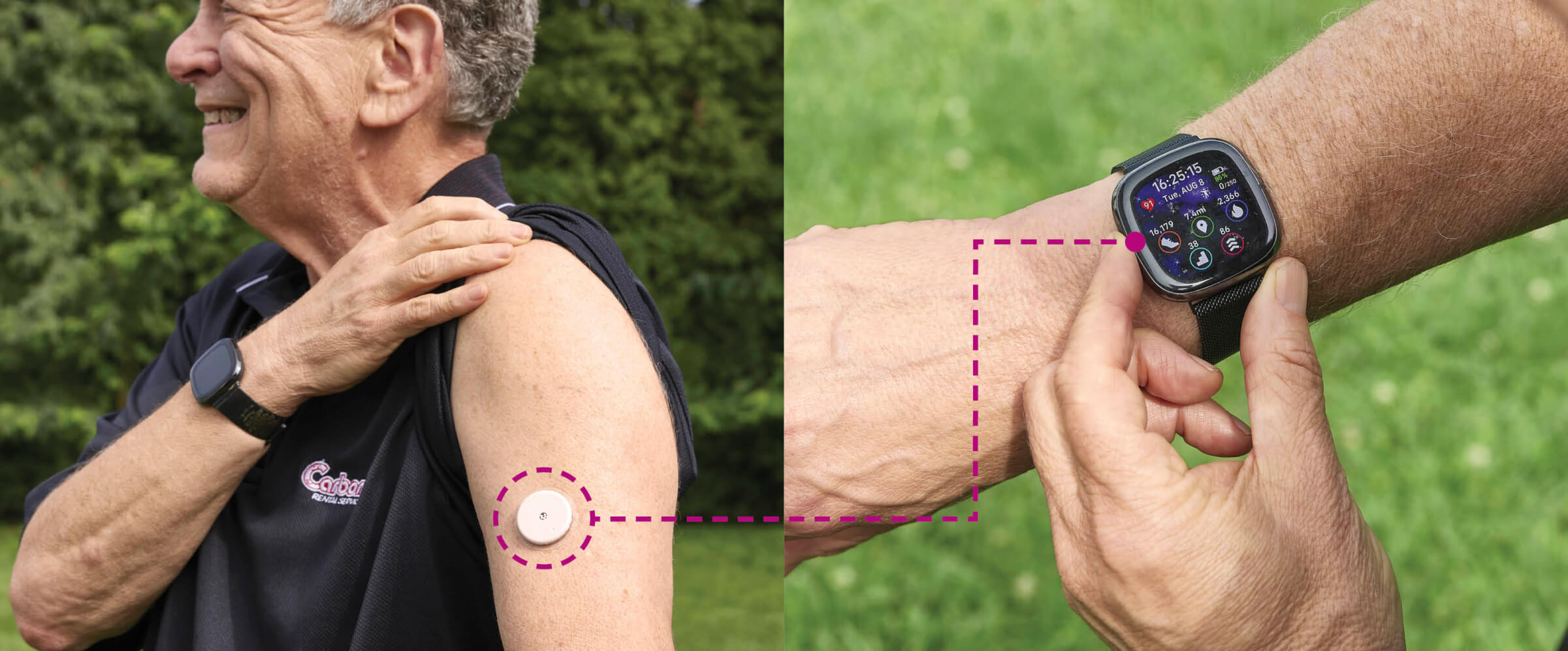
But earlier this year, Medicare expanded coverage for continuous glucose monitors (CGM), making it significantly easier for Pincus, 70, and millions of others to manage their blood sugar levels. Once used mostly for insulin-dependent type 1 diabetes, CGM use is rising fastest in people like Pincus with type 2 who typically take oral medications and may use injectable drugs, sometimes along with insulin, to control blood sugar.
To better manage his diabetes, Pincus wears a patch with a glucose sensor on his upper arm that transmits blood sugar (glucose) data to his smartphone. “I take readings several times during the day. When I see spikes and valleys, I think about what I ate that caused that. I’ve lost weight and my A1c [a 90-day blood sugar average] is lower.”
Experts estimate the Medicare rule change makes 1.5 million more older adults eligible for the devices, many with type 2; if private insurance plans follow suit, another 2.5 million people, almost all with type 2, will have insurance coverage. The change is one reason analysts say by 2027, at least 5.9 million people with type 2 diabetes will be eligible for insurance-covered CGMs. That could grow to 8.4 million if private insurers also expand coverage. “This is great news for patients with type 2 diabetes,” says Tamara Oser, M.D., who studies CGM devices at the University of Colorado Anschutz Medical Campus in Aurora.
Compared to finger-stick blood sugar checks, CGM devices help midlife and older adults lower their blood sugar further and keep it in a healthy range longer. In Oser’s recent pilot study that used CGM with a lifestyle guide and Fitbit, 67 percent of newly diagnosed type 2 patients obtained diabetes remission. Oser is also testing CGM in prediabetes, which almost 64 million midlife and older Americans have.
Meanwhile, Pincus has used his CGM to see how certain foods, as well as sleep and stress, affect his glucose levels. “CGM has the ability to change lives,” he says.
MORE DIABETES BREAKTHROUGHS

App Helps You Stay on Track
A prescription-only smartphone app, which uses cognitive behavioral therapy techniques to help people with diabetes develop new habits, received FDA authorization in July. People using the AspyreRx app for 90 days saw their A1c, a measure of long-term blood sugar control, fall significantly.
Diabetes Drug Sparks Weight Loss
In May 2022, the FDA approved tirzepatide (Mounjaro), an injectable diabetes medication that activates receptors on cells for glucose-controlling hormones. The drug also helps with weight loss; after approval, some dosages were in short supply as people with and without diabetes flocked to fill prescriptions.
ON THE HORIZON
ARTIFICIAL PANCREAS FOR TYPE 2 DIABETES
► In January 2023, a small British study showed that an experimental “artificial pancreas”—a device that measures blood sugar continually and releases insulin into the bloodstream as needed—was more successful at lowering blood sugar than standard insulin injections for adults with advanced type 2 diabetes. Researchers say larger studies are needed to fully test the device.
BREAKTHROUGHS IN
MEN’S HEALTH
Cancer Treatment From Inside the Prostate Gland

Tommy Saul with his wife, Autumn
TOMMY SAUL, 57, takes prostate cancer seriously. His father died after a 12-year fight with the disease, the second-leading cause of cancer death in men. So when Saul’s annual prostate specific antigen test (a measure of prostate health) showed that his PSA levels had doubled, and a biopsy in 2022 confirmed that he had prostate cancer himself, his doctors urged radiation or immediate surgery to remove his prostate gland. Still, despite his family history, Saul hesitated. “I didn’t like the side effects—urinary incontinence and erectile dysfunction,” Saul says. “But I wanted to live a long time for my wife and our three sons. That’s when we did a lot of research.”
Saul and his wife, Autumn, decided that he was a good candidate for TULSA-Pro, an outpatient procedure cleared by the FDA in 2019 that destroys cancerous tissue from inside the prostate gland with ultrasound heat. Doctors use magnetic resonance imaging to guide the robotic procedure while a cooling catheter inserted in the rectum reduces heat exposure of nearby tissue. Recovery is generally faster than with surgery or radiation. It’s intended mostly for men with low- and intermediate-risk prostate cancer that hasn’t spread.
“The goal is to minimize side effects,” says Yair Lotan, M.D., chief of urologic oncology at the University of Texas Southwestern Medical Center, in Dallas. “We can’t guarantee a risk-free experience. But with magnetic resonance imaging to guide the procedure, we can be very precise.”
In a recent study of 115 midlife and older men with low- to intermediate-risk prostate cancer who had their prostate gland completely treated via TULSA-Pro, 96 percent of participants saw their PSA levels fall by 75 percent or more within a year, 25 percent had new problems with erectile dysfunction (ED), and 11 percent reported some urinary leakage or incontinence.
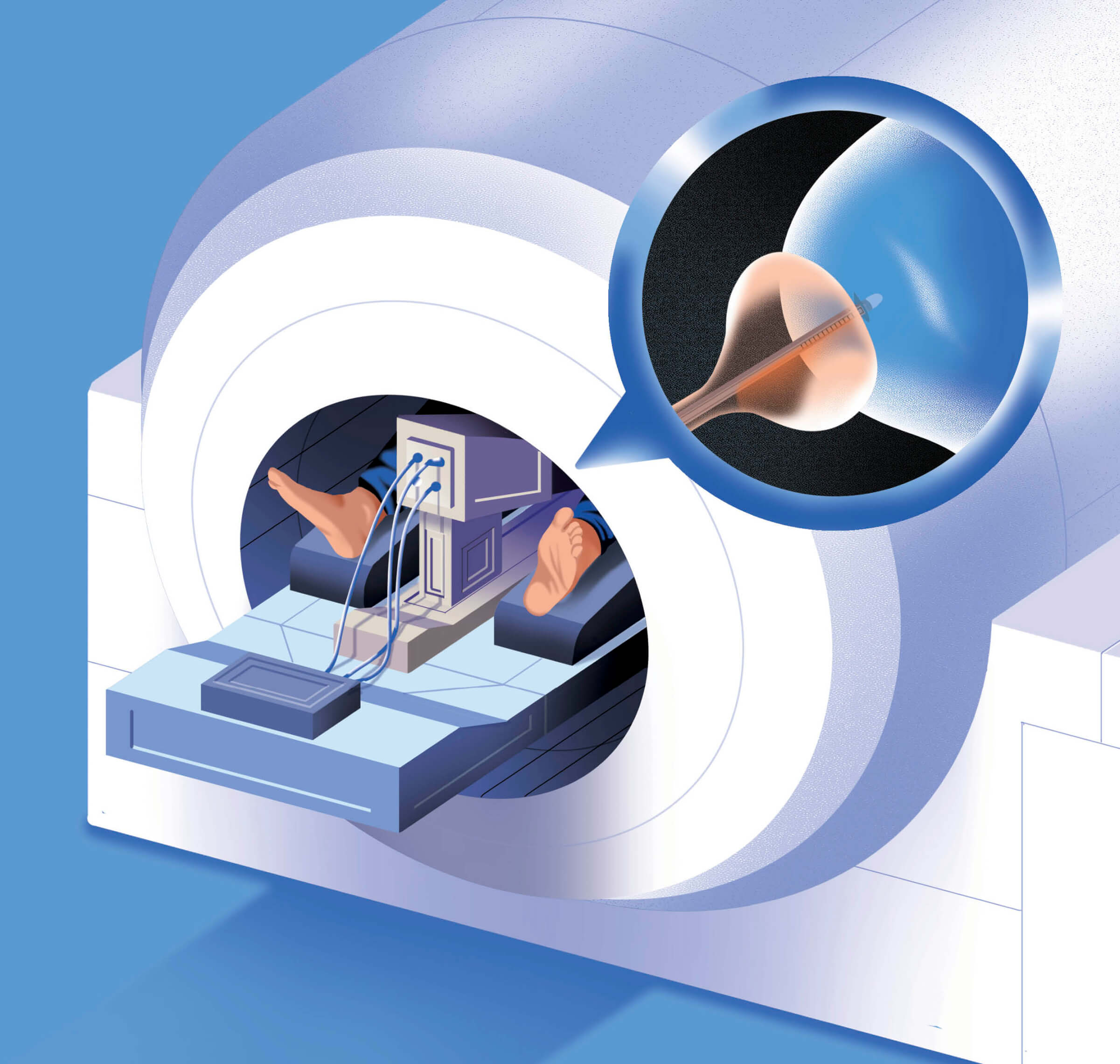
The TULSA-Pro procedure treats prostate cancer with minimal side effects.
By three years after their procedures, 13 percent needed additional prostate cancer treatment, but none had severe erectile problems, and 99 percent didn’t need pads for managing incontinence.
In contrast, 25 percent to 33 percent of men who undergo standard surgery or radiation treatment see their cancer return, according to the Prostate Cancer Foundation. Up to 23 percent may have lingering incontinence after surgery, and up to 50 percent may have ongoing ED a year or more after surgery or radiation. These side effects can dramatically affect a man’s quality of life.
Lotan says ultrasound and other “focal” cancer therapies that treat part of the prostate are active areas of research offering new hope to men with prostate cancer. “Twenty years ago if you had prostate cancer, it was surgery or radiation,” he says. “Now focal therapy is an evolving area.”
Saul says he’s had no incontinence or erectile dysfunction since his TULSA procedure at the Ronald Reagan UCLA Medical Center, in Los Angeles, in August 2022. “I travel a lot for my job, on jets without restrooms,” he says. “And my wife and I have a passionate relationship. We didn’t want to lose that.”
Follow-up tests show his PSA levels have dropped from 12 to 3, an encouraging sign, and MRI scans of his prostate haven’t found any trouble spots or signs of cancer.
“At a different stage of life or a different stage of cancer, surgery or radiation might have been the best option,” Saul says. “But this was perfect for me.”
MORE MEN’S HEALTH BREAKTHROUGHS


Over-the-Counter Help for Erectile Dysfunction
A nonprescription gel that helps men get an erection within 10 minutes received FDA clearance in June. Eroxon, already sold in Europe, stimulates nerves involved with erections by cooling then warming the penis, which makes blood vessels dilate, according to maker Futura Medical. It’s effective for 65 percent of people who try it, the company says.
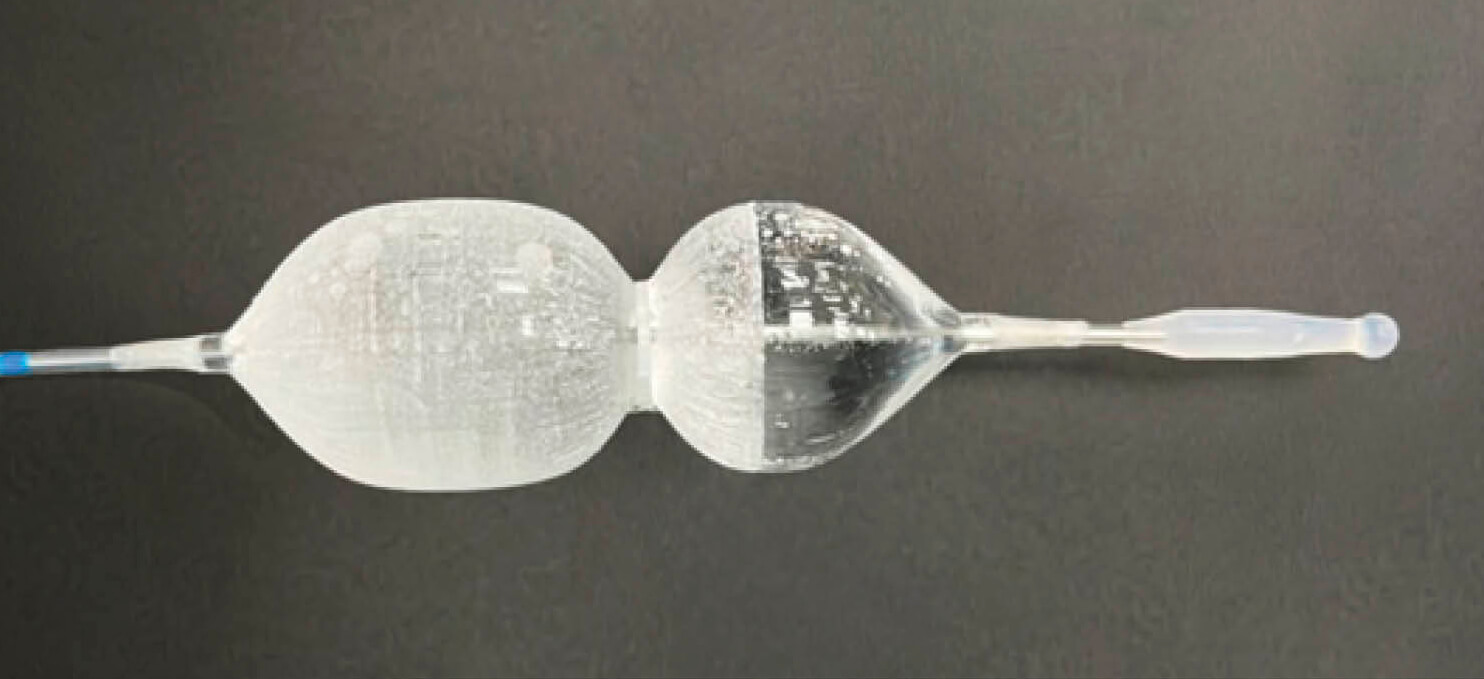
New Treatment for Relieving Symptoms of Prostate Enlargement
A new catheter system approved by the FDA this past June treats troublesome urination problems caused by benign prostatic hyperplasia (BPH)—an enlarged prostate. The Optilume BPH Catheter System is a drug-coated balloon that expands in the prostate gland opening, enlarging it to allow for the flow of urine. At the same time, the device releases the medication paclitaxel to help prostate tissue heal. Men with BPH often have to pee repeatedly and urgently, and may have difficulty starting a stream of urine or experience a weak flow. Those who underwent the new catheter procedure not only increased their urinary flow rate by more than 70 percent, but they were still reporting urinary improvement four years later, according to a 2023 study of 80 subjects.
ON THE HORIZON
LAB-GROWN HAIR FOLLICLES FOR BALDNESS
► Japanese researchers have grown hair follicles in a lab by reprogramming mouse cells, and most sprouted hairs that grew to about a 10th of an inch long. In the future, the follicles could be used to test hair-loss treatments, they say.
BREAKTHROUGHS IN
BRAIN HEALTH
Nerve Stimulation for Stroke Recovery

Mild electrical pulses help boost the effectiveness of stroke-recovery therapy.
A 2020 STROKE caused by a blocked artery on the left side of her brain left Kathy Reynolds, 69, unable to use her right hand. Despite extensive rehab, she couldn’t knit or even cut her own food. “I learned to do things with my left hand and tried holding one knitting needle under my armpit,” says this retired teacher from Succasunna, New Jersey. “But there were things I just couldn’t do.”
In February of this year, Reynolds had a new type of device implanted just below her collarbone, with a wire under the skin leading to her vagus nerve. During occupational therapy sessions and at home, she or her therapist can turn on the Vivistim System, sending mild electrical pulses to the vagus nerve and on to the brain. Stimulating the vagus nerve changes electrical activity and levels of neurotransmitters in brain cells, nudging the brain’s efforts to build new pathways as Reynolds works to recover the use of her right arm and hand.
Long used to quiet seizures for people with epilepsy and for stubborn depression, vagus nerve stimulation (VNS)—paired with extensive rehab—helped people recover more use of their arms and hands in a recent study of 108 stroke survivors published in The Lancet. Up to 60 percent of stroke survivors have lingering problems with use of their hands and arms. “The conventional wisdom up until now is that by a year after a stroke, there really isn’t much that helps,” says study coauthor Charles Liu, M.D., director of the Neurorestoration Center and professor of neurological surgery at the University of Southern California Keck School of Medicine. But with VNS, “it is possible to achieve meaningful improvements many years after stroke,” the study’s authors conclude.

Kathy Reynolds is regaining use of her right hand.
It takes hard work. People in the study completed an intensive rehab program of three 90-minute in-clinic sessions per week for six weeks, plus additional sessions at home, repeating the hand and arm movements needed for everyday tasks—such as grabbing, eating and opening containers—hundreds of times. Those who did just the rehab program recovered some additional use of their arms and hands, but adding VNS doubled the amount of improvement. “The vagus nerve connects many parts of the body to many parts of the brain,” Liu notes. “It’s a natural antenna.” The system helped about half of users. “In general, people have been happy with their improved level of function,” Liu says. “It’s important to understand that VNS is not a panacea; not all your stroke symptoms will be gone.”
In 2021, the FDA approved Micro-Transponder’s Vivistim System, which pairs VNS with hand and arm rehab in people who’ve had an ischemic stroke (the most common type, caused by a blood vessel blockage). Vagus nerve stimulation is the topic of continued medical research. In the future, VNS and other types of nerve stimulation may be used to jumpstart recovery of mobility in legs and feet, too, Liu notes. VNS lab studies have also looked at VNS’s effects on thinking and memory after a stroke.
Meanwhile, Reynolds recently succeeded in writing with a regular pen, rather than one with a large foam grip, with her right hand. And she’s using both hands to knit—including a practice piece with a checkerboard pattern. After a short walk with her best friend, the two women sit together like old times.
“We visit, we chitchat, we knit,” she says. “There are pathways in my brain that haven’t been working since my stroke. This is making them wake up again.”
MORE BRAIN HEALTH BREAKTHROUGHS
Cerebrospinal Fluid Tests for Alzheimer’s Disease
New tests that measure beta-amyloid and tau proteins in cerebrospinal fluid—which surrounds the brain and spinal cord—could help doctors diagnose early Alzheimer’s so people with the disease can take new and emerging medications that may slow progression. One test, cleared by the FDA in 2022, compares levels of two beta-amyloids that build up in the brain with Alzheimer’s. Other tests for Alzheimer’s biomarkers have also received FDA clearance in the past two years. In studies, results of the tests were comparable to PET brain scans used to detect Alzheimer’s brain changes.
Magnetic Brain Stimulation for Mental Health Disorders
Transcranial magnetic stimulation (TMS), first cleared by the FDA for treatment-resistant depression in 2008, shows promise for a wide variety of mental health conditions, including anxiety, post-traumatic stress disorder and addiction. It uses magnets to stimulate brain cells. Conventional TMS requires six weeks or more of daily sessions, but the SAINT system, a new version of accelerated TMS, received FDA clearance in 2022. One study of people with treatment-resistant depression showed a remission rate of 79 percent after just five days of using SAINT.
ON THE HORIZON
SMARTWATCHES THAT CATCH EARLY PARKINSON’S
► Researchers analyzed data from 103,712 people who wore a smartwatch-like movement-tracking device for a week. Those who went on to develop Parkinson’s disease after wearing the watch showed signs of a unique slowness of movement up to seven years before diagnosis. Researchers say the finding could help detect this neurological disorder earlier and possibly aid in prevention studies.
Sari Harrar is a contributing editor to AARP THE MAGAZINE.