Staying Fit

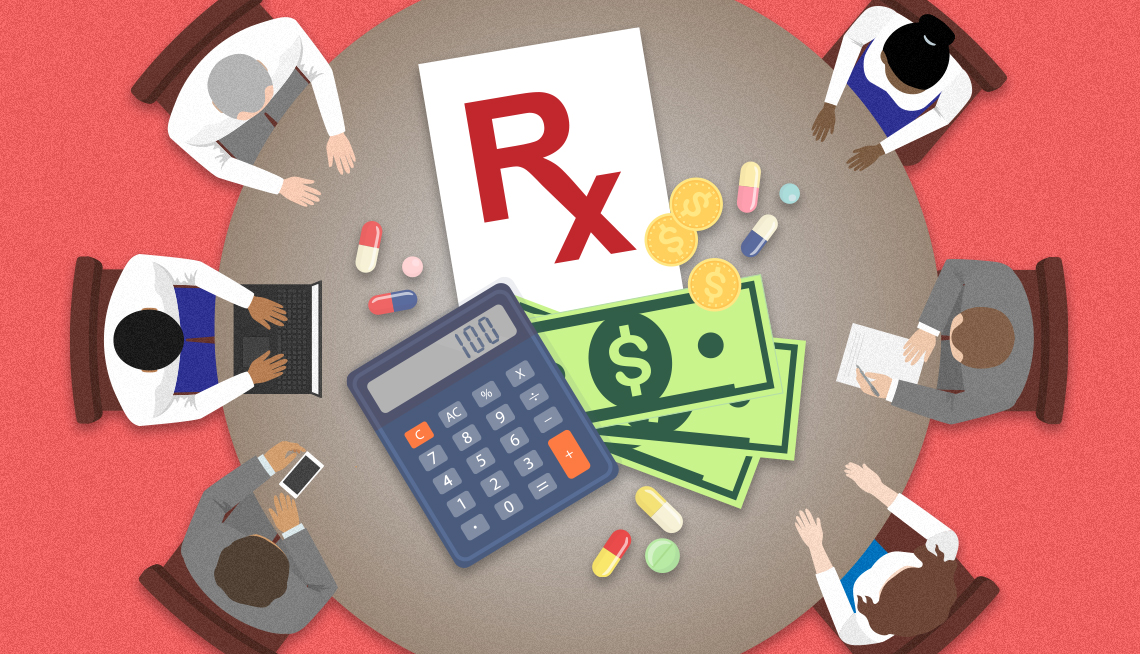
The conversation continues between Medicare and the makers of the first 10 prescription drugs whose prices the federal government has the power to negotiate for the first time in history.
Included in this first batch of medications whose prices are being negotiated as part of the new prescription drug law are life-sustaining therapies that millions of older Americans in the nation’s largest health program rely upon to prevent strokes and blood clots and to treat diabetes and cancer.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
The U.S. Department of Health and Human Services (HHS), which started price negotiations with drug manufacturers in February, has received counteroffers to its initial proposals and has invited all 10 of the drugmakers to “participate in further discussions.”
Negotiations are expected to continue over the next few months and are scheduled to conclude in August. New prices for those medications agreed to by the federal government and the drugmakers will take effect in 2026.
“This is an important first step toward finally allowing Medicare to use its purchasing power to lower drug prices,” Nancy LeaMond, AARP executive vice president and chief advocacy and engagement officer, said when the 10 first drugs were announced in August. “Medicare spends more than $135 billion on prescription drugs every year.”
Between June 2022 and May 2023, Medicare Part D spent $50 billion on the first 10 drugs selected for negotiation. That represents 20 percent of Part D spending during that time period. These medications were used by 8.2 million Medicare beneficiaries.
In the long run, Medicare beneficiaries, who often must pay a percentage of a drug’s cost, would benefit directly from lower negotiated prices, and the government could use the money saved to shore up Medicare’s finances. Negotiations will be expanded to include additional drugs in the years ahead, which will magnify the savings. Lower Medicare spending is also expected to lead to lower Part D premiums.
“Letting Medicare negotiate for lower prices is a commonsense solution that will save seniors money and cut government overspending,” LeaMond says.
How the drugs were picked
Under the Inflation Reduction Act, the government was required to make public by Sept. 1, 2023, the 10 medications covered by Medicare Part D that comprise the first round of the price negotiation process.
To be eligible for negotiation, medicines that are called small molecule drugs — those you typically get at the pharmacy and take in pill form — must have been on the market for seven years and not have a generic alternative. Biologics, which are drugs made from living organisms rather than chemicals, must have been available for 11 years with no nearly identical alternatives, known as biosimilars, on the market.
Federal officials drew the list of 10 drugs from among the 50 medications that Medicare Part D spends the most on and that are used most by beneficiaries. All but three are small molecule medicines. Drugmakers that decline to negotiate prices face substantial financial penalties or must stop participating in Medicare and Medicaid, the health coverage program for people with low incomes.


















































































More From AARP
10 Prescription Drugs That Cost Medicare the Most
Blood thinners, diabetes treatments dominate the latest list of costliest Part D medications
AARP Urges Court to Keep Drug Price Negotiations on Track
Delaying the new law would harm older Americans, legal brief saysWhat You Need to Know About the Medicare Insulin Cost Cap
Get answers to common questions about the new law