AARP Hearing Center


About a quarter of women ages 50 to 74 are not up to date on routine mammograms despite pleas from doctors and public health experts that more middle-aged and older women get screened for breast cancer. A new study from federal researchers pinpoints several factors that are causing women to skip out on screenings — and it’s not just cost and access to health care.
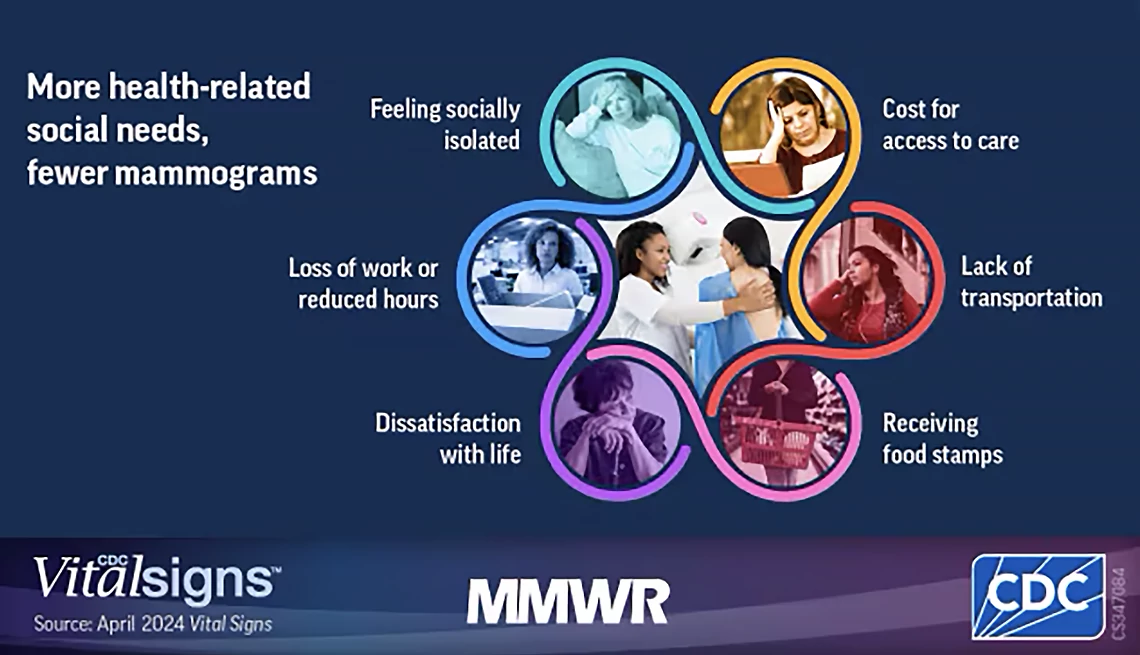
Feeling socially isolated, experiencing food insecurity or job loss, or not having access to reliable transportation can affect mammogram participation, according to a study published April 9 from the Centers for Disease Control and Prevention (CDC). Another so-called health-related social need that keeps women from getting screened is a general dissatisfaction with life.
“If we are to achieve higher breast cancer screening for all women, we have to look at all the possible challenges women face in getting mammograms,” Lisa C. Richardson, M.D., director of the CDC’s Division of Cancer Prevention and Control, said in a news release.
Researchers analyzing data from the 2022 Behavioral Risk Factor Surveillance System found that the more health-related social needs a woman has, the less likely she is to get a mammogram. About 83 percent of women with no health-related social needs had received a mammogram in the previous two years, compared with about 66 percent of those with three or more health-related social needs. The cost of health care was the biggest barrier, the study found.

“The bottom line is, women are more likely to get lifesaving mammograms when their social needs are met,” Jacqueline Miller, M.D., medical director of the CDC’s National Breast and Cervical Cancer Early Detection Program, said in a news briefing.
Breast cancer, which can also be diagnosed in men, is the most common cancer among women in the U.S., and a 2024 report from the American Cancer Society shows its incidence is increasing. The disease claims more than 42,000 U.S. lives each year, and a disproportionate share of these deaths are among Black women. The median age of a breast cancer diagnosis in women is 63. However, screening with a mammogram — an X-ray picture of the breast — can reduce cancer deaths, research suggests. A Swedish study published in the journal Cancer found a 41 percent reduction in fatal breast cancers within 10 years of diagnosis among women who participated in mammography screenings.
New draft guidelines from the U.S. Preventive Services Task Force recommend that women start getting regular mammograms at 40, rather than 50, and continue with them every other year through age 74. Public comments on the draft recommendations end June 5, after which final guidelines will be issued.































































More From AARP
AARP Smart Guide to Keeping Your Memory Sharp
22 science-backed ways to growing a healthier, happier brain, now and in the future
Medical Breakthroughs in Women’s Health
Advancements include new scans for dense breast tissue, help for hot flashes and more
6 Things Women Wish Their Doctors Told Them About Turning 50
Here are some of the big changes you should expect and what you can do about each oneFDA Approves New Treatment for Hot Flashes
The pill expands options for people going through menopauseRecommended for You