AARP Hearing Center

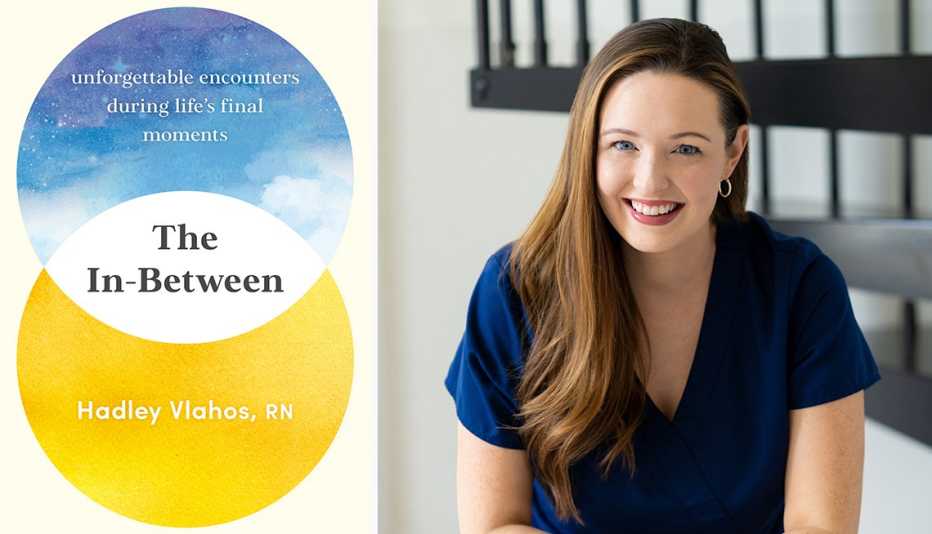
For anyone who has ever wondered about hospice care for themselves or for a loved one, Hadley Vlahos, an RN and six-year registered hospice nurse, has written The In-Between: Unforgettable Encounters During Life’s Final Moments. The book features her heartfelt reflections on her most impactful experiences with her hospice patients. Vlahos, 30, whose social media outreach about hospice care has amassed her more than a million followers, shares her insights on an often-taboo topic that warrants more open discussion.
Why did you write this book?I started sharing my stories about being a hospice nurse on social media three years ago. I was shocked how it resonated with people. Many don’t want to talk about hospice or death or dying. One day I got a direct message from someone who was at the bedside of her dying husband. She said that she had been watching my social media videos and that I brought her peace. She felt like I was there at his death. That’s when I decided that a book could go way deeper than a 60-second video.
Who is the book for?
It’s for anyone who has lost a loved one or is going through grief or is considering hospice. It’s also for anyone who is fearful of death.
Why did you decide to become a hospice nurse?I did not start in hospice. I did an externship in a hospital where I did everything from delivery to immediate care. Then I became a nursing home manager. That’s where I saw hospice care for the first time. I was managing 40 patients. I would watch hospice nurses come in and sit one-on-one with their patients for a while. I said to myself, that’s what medicine is supposed to be like. I became a hospice nurse.
What’s the best part about being a hospice nurse?The best thing by far is the relationships. You are in people’s homes and surrounded by their memories, like all the pictures on the wall and their pets. You get to know people at a different level and you get to know them for many months.
What’s the worst?The worst thing is that there is a nursing shortage in every field. Hospice is 24/7, so it can be difficult to work all day, cover (for someone else) all night, then work the next day. It can be draining.
How do your patients approach the end-of-life process?People go through stages. Sometimes they are very resistant to going to hospice. We try to start slow and let them get to know us. They often go through a life review and become a bit more accepting. They talk about what they did well; what they wished they’d done. They accept the decline. Our bodies know how to die. Usually, people are at peace at the end.
It must be difficult getting close with patients you know will eventually pass on.
It’s not always easy. From what I’ve seen as a hospice nurse, I firmly believe that when people die, it’s not the end. I know it may be a while, but I believe I’ll see them again. This won’t be the last time I see them.
































































More on Caregiving
What I Learned From My Mom’s Approach to Death
Final months filled with grief, gratitude and life lessons
Nontraditional Burial Options Can Spur End-of-Life Conversations
A ‘gradual goodbye’ process can ease caregiver stress, aid acceptance
What to Do When a Loved One Dies
Practical steps you need to take in the early days