AARP Hearing Center


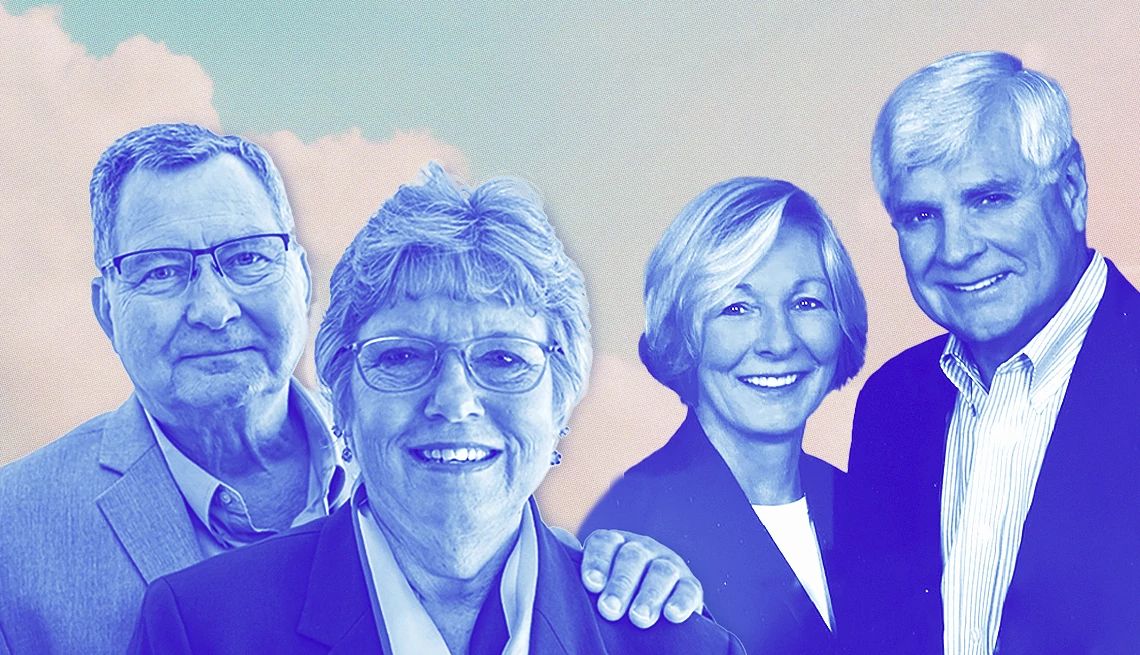
Don Young and his wife, Kay, of St. Charles, Missouri, are not always on the same page when it comes to protecting his health after five heart artery stents and a heart valve replacement.
Kay, 75, would like Don, 80, to eat less salt — but Don still eats potato chips. Kay would like Don to listen to his doctor and stop doing lawn work on hot days. Don says when his lawn needs mowing, he does it.
But Don says he does value Kay’s caregiving — including the many hours she’s spent with him in hospitals, tracking every drug and procedure and, he says, warding off disaster. She’s helped him through 31 years of health challenges that started with throat cancer and got more complicated when he developed coronary artery disease nearly 20 years ago.
Don, who speaks with a device called an electrolarynx, says: “If it wasn’t for my wife, I’d be dead.”
When someone has coronary artery disease — the kind of heart disease that is usually caused by blocked arteries and can lead to chest pain, heart attacks, and other complications — family caregivers can make a big difference, research suggests.
“People who have a lot of support from their family actually recover better, they recover faster, and they do better long term,” after a crisis like a heart attack, says Vinoy Prasad, M.D., director of interventional cardiology and cardiac rehabilitation at Loma Linda University International Heart Institute in California.
So, if you care for someone with coronary artery disease, which is sometimes called coronary heart disease, here’s what you can do to support them.
Learn about coronary artery disease
Your coronary arteries, which wrap around and branch into your heart, deliver oxygen-rich blood to the heart muscle. When that blood flow is reduced, you can get symptoms like chest pain, shortness of breath, and fatigue. When the flow stops or is severely restricted, depriving the heart of oxygen, that’s a heart attack.
The most common cause of coronary artery disease is atherosclerosis, or the buildup of plaque in arteries. Plaque is a sticky substance made of fats, cholesterol, calcium, and other substances. It can build up over many years, narrowing arteries and reducing blood flow. A complete blockage sometimes happens when a piece of plaque breaks off and produces a blood clot.
Learn the Signs of Heart Attack
Anyone with coronary heart disease is at risk for a first or repeat heart attack. Here are some possible signs, from the American Heart Association:
- Pain, pressure, squeezing, or fullness in the chest.
- Pain or discomfort in one or both arms, the back, neck, jaw or stomach.
- Shortness of breath, with or without chest discomfort.
- Other signs such as nausea, vomiting, lightheadedness, and cold sweats.
- When you see the warning signs, call 911. An ambulance crew can start treatment if needed.
High levels of unhealthy cholesterol, high blood pressure, smoking, diabetes, obesity and a family history of the condition raise your risk for this kind of heart disease, according to the American Heart Association.
Some less common types of coronary artery disease, called nonobstructive coronary artery disease, include damaged artery linings and artery spasms that restrict blood flow without plaque buildup.
Too many people find out they have coronary artery disease only when they have a heart attack, says Seth Martin, M.D., a cardiologist and professor of medicine at Johns Hopkins University. Others, he says, find out when symptoms lead them to get a CT scan called a coronary angiogram that can show narrowed arteries. Cardiac catheterization, where a long, thin tube is threaded through blood vessels, dye is injected, and then an X-ray is used show any blockages, can also diagnose the condition.
With catheterization, routinely done after a heart attack, the blockages can be fixed right away, often by widening the artery with a mesh tube called a stent. In some cases, bypass surgery is needed to make a new path for blood around the blockage.
If your loved one has a heart attack today — and gets to a hospital quickly — they stand to benefit from “a tremendous evolution" in care, that has greatly improved survival and lowered the risk of repeat heart attacks, Martin says. Fast reversal of blockages can limit heart damage, he says.
Today’s medications, which include many drugs to lower cholesterol and blood pressure and to improve heart function, also are extending lives, Prasad says.










































































More From AARP
Help! My Doctor Won’t Listen to Me
Adam Rosenbluth, M.D., gives advice for getting your physician to really pay attention to youHow to Be a Caregiver for Someone With Chronic Kidney Disease
Consistent medical monitoring and a healthy diet can make a big differenceHow to Be a Caregiver for Someone With COPD
Care for a COPD patient at home and improve their quality of life