AARP Hearing Center

I remember being on a treadmill when I was 51 and randomly watching a TV ad for vaginal estrogen. Ding, ding, ding. So that explains my sore vagina.
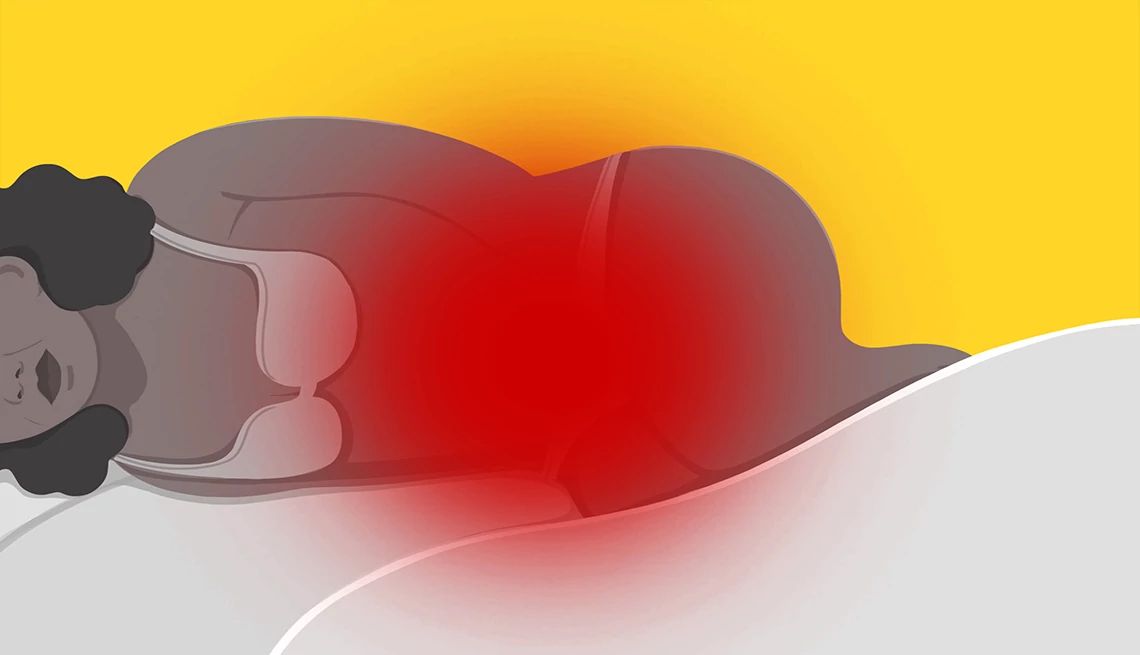
In this week’s column, our sexual health experts shine a light on the vaginal pain that many 50-plus women experience during sex. Yes, it’s normal — and, no, it doesn’t have to hurt.


In the Mood
For AARP’s In the Mood column, writer Ellen Uzelac will ask experts your most pressing 50+ sex and relationship questions. Uzelac is the former West Coast bureau chief for The Baltimore Sun. She writes frequently on sex, relationships, travel and lifestyle issues.
We also tackle a reader’s question about sex following a prostate cancer diagnosis. After skin cancer, prostate cancer is the second most diagnosed cancer in the U.S., according to the Prostate Cancer Foundation. And the older you are, the greater your chance of developing it.
At 52, sex has become uncomfortable and burns afterward. Is this normal?
“One of the most important things to talk to patients about is this whole idea of normal. Yes, it’s part of aging ... but if you’re uncomfortable, we can do something about it,” says Anita Mikkilineni, an ob-gyn focused on sexual health at George Washington University Medical Center in Washington, D.C.


LIMITED TIME OFFER: Labor Day Sale!
Join AARP for just $9 per year with a 5-year membership and get a FREE Gift!
First, a quick tour of the vagina. Estrogen helps keep the tissue of the vagina and the entrance to the vaginal canal plump, moist and supple — a happy place, one hopes, for your partner’s penis. With the onset of menopause, which typically occurs in your early 50s, Mikkilineni says estrogen levels decrease, often causing dryness that can make penetrative sex painful.




























































You Might Also Like
Can a Sexless Marriage Be Saved?
A man considers intimacy outside of a sexless marriage. And a woman dislikes sex
Does Exercise Affect Sex Drive? And How Can I Prevent Premature Ejaculation?
Experts answer the questions you are too embarrassed to askQuiz: Test Your Pain-Free Sex IQ
Sex as a 50+ adult can sometimes be painful. Take this quiz to learn how to make it pain-free and enjoyable
Recommended for You