7. Long naps
“Many adults don’t nap voluntarily or intentionally, but often fall asleep when not busy or watching TV,” says Doghramji. Either way, your brain sees it as sleep. The most common time of the day when people get sleepy is between 2 and 3 in the afternoon, when we experience a natural dip in energy, he says. This may prevent you from feeling tired at bedtime; then spending too much time lying awake can contribute to insomnia. If your afternoon energy tends to be low, try scheduling something active for that time instead of napping. It will help you feel refreshed, and research shows that exercisers have better sleep quality too — so it’s a double bang for your buck.
If a nap calls your name, Pelayo suggests sleeping no longer than 40 minutes to avoid feeling groggy later. Rest your head where you normally sleep so you remain accustomed to the same sleep environment.
8. Spending too much time in bed
Reading may be a relaxing activity but you should take your book to an armchair — not your bed, Harris advises. “I prefer that the bed is only used for sleep and sex,” she says. Even calm activities like puzzles or an adult coloring book can cause your brain to associate the bed with activities that you pursue while awake, which can affect your ability to drift off at night.
9. Alcohol
Yep, a glass of vino can simmer you down and make it easier to fall asleep. However, research shows that while it may help you conk out, there’s also a rebound effect that causes lighter and more fragmented sleep in the second half of the night; that’s why you’re up at 3 a.m. It also decreases sleep quality — so you rise less refreshed.
Limit alcohol to three hours before bedtime and imbibe moderately (one drink for women and two for men, as recommended by the Centers for Disease Control and Prevention).
10. Medications
Sleep can also be interrupted by poor timing of your medications. Some, like diuretics for blood pressure, can make you have to urinate more often. More than one or two bathroom breaks at night is abnormal, Doghramji says.
Antidepressant SSRIs, can either be energizing or sedating, depending what type you’re on. Steroids like prednisone, beta blockers like propranolol and certain asthma medications are best taken in the morning to avoid sleep disruptions. Always consult your doctor before changing the timing of your medication. See "Common Medications That Can Affect Sleep" for more details.
11. Stress
Dealing with stress can make falling asleep difficult, leading to light, fragmented sleep. However, there are tools to help alleviate stress-related insomnia.
For example, if you’re stressed over bills, avoid reviewing or addressing them in your bedroom. “Put it in a separate room so when you go to your room, it’s a different world,” says Pelayo who also wrote How to Sleep: The New Science-Based Solutions for Sleeping Through the Night.
If you have persistent thoughts that trap you in a cycle of negative feelings, schedule a dedicated time to think or worry. Consider journaling or writing a simple list, whether it’s what you need from the grocery store or even jotting down short- and long-term goals.
“Say it and believe it, then put that aside,” says Pelayo. "Now do something that you enjoy. Reach for pleasure, a warm bath or time with your spouse.” These activities can be incorporated into your sleep routine to signal to your body that you are transitioning into sleep mode and the day is over.
Problems may seem less intense in the morning than they do at night.
Finally, cognitive behavioral therapy for insomnia (CBT-I), can help you retrain your thoughts to calm your mind, Doghramji says. A specially trained CBT-I therapist can help, but there are also apps that teach you these important skills. “Don’t just use them at 3 a.m.; practice with these apps during the day.”
12. Forced-sleep
As you get older you may start going to bed earlier but you may want to consider pushing it back later.
“You want a later bedtime, but a locked in wake-up time. That’s going to squeeze out those middle of the night awakening… and the body’s going to sleep deeper,” says Pelayo.
Lying in bed trying to force sleep to happen out of boredom backfires, Harris says. It can convince your brain that being awake in bed is normal. Instead, get up and go into a different room and do something relaxing and calm in dim light, she advises. (No screens allowed.) Having an accepting mindset about it can also help. “Sleep will come when it comes. If not tonight, don’t sleep in to compensate — and you’ll likely sleep better the next night,” she says.
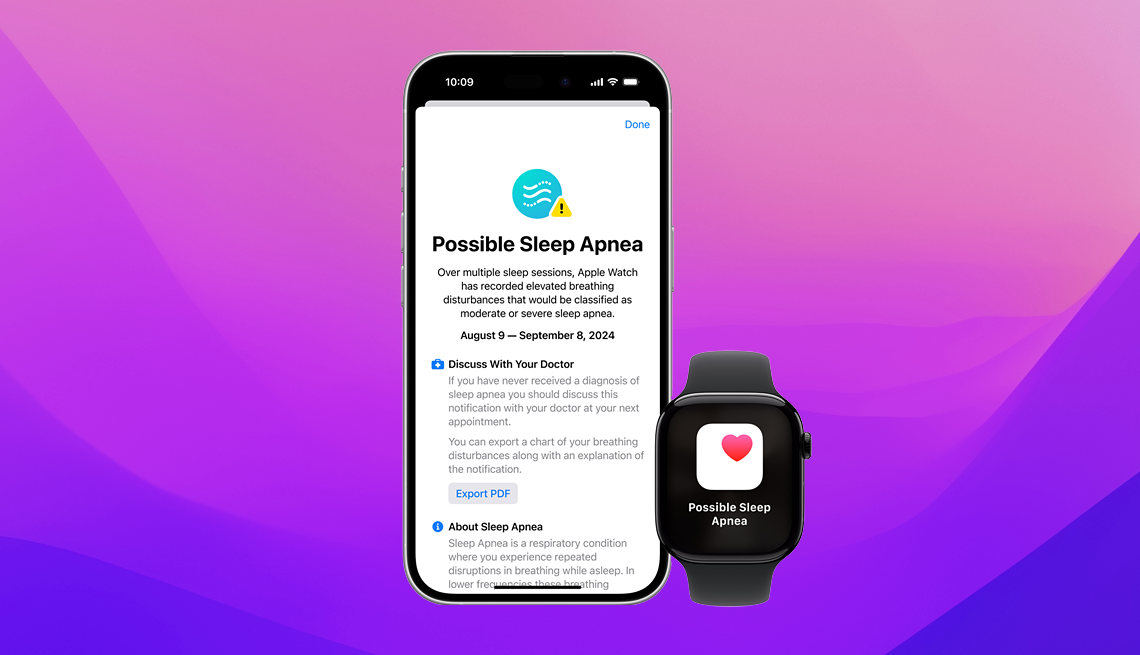
13. Health condition affecting sleep
“Insomnia is both a symptom and a disease,” says Watson. If correcting your sleep habits hasn’t improved its quality, your insomnia may be a symptom of another condition.
There are over 80 sleep disorders, many which include insomnia as a symptom. These include sleep apnea, restless leg syndrome, parasomnia (such as sleepwalking, talking or eating) and narcolepsy. While a relatively rare condition, older adults in particular are susceptible to REM sleep behavior disorder (RBD), where individuals physically act out their dreams while asleep. This not only may cause injury to oneself or their bed partner but can be an early warning sign of Parkinson’s, Lewy body dementia or multiple system atrophy, a rare neurodegenerative disorder that affects the body's involuntary functions, and should be treated by a doctor.
Other non-sleep disorders that may cause insomnia include pain, arthritis, atrial fibrillation, PTSD and heartburn, according to Pelayo.
If you’ve tried the correcting your sleep on your own for a month and it still doesn’t feel adequate, see your doctor for an evaluation.
14. Exercising too close to bedtime
Exercise offers numerous benefits for better sleep, such as reducing anxiety and depression and realigning your circadian rhythm. But working out too close to bedtime may be counterproductive. Exercise can heat up your body or make you feel more alert which can make it harder to sleep. Instead, aim to exercise at least two hours before bed to allow these effects to wear off.
Treatment options for insomnia
Cognitive behavioral therapy for insomnia (CBT-I): This is typically recommended as the first-line treatment because it identifies and addresses habits, behaviors, thoughts and other factors that keep you awake during the night. Think of it as getting a toolbox for overcoming insomnia.
Medication: Those who opt for medication should know that there can be side effects and limitations for long term use. For older adults, sleeping pills can be especially dangerous due to the risk of mobility problems and falls. However, if you’re dealing with temporary insomnia, your doctor might give you a short-term prescription.
Alternatively, a relatively new category of medication called dual orexin receptor antagonist (DORA) has proven to be well tolerated in older adults with insomnia and can be a good alternative to traditional prescription sleeping pills.
Over-the-counter options: In general, it’s best to steer clear of over-the-counter options like melatonin, Tylenol PM or Advil PM. They may not provide the most effective solution and could mask an underlying medical condition responsible for insomnia, which might require a doctor’s evaluation, says Watson. “If you’re just addressing the insomnia yourself over the counter, you might miss an opportunity to address the root cause.”
Alcohol: While alcohol may help you fall asleep initally, as it wears off, your sleep becomes more disrupted toward the last half of the night.
Cannabis: The role of cannabis in promoting sleep remains uncertain, and its potential effects are still being researched.
When to see a doctor
You should reach out to a doctor when insomnia begins to impact your daytime function or if you routinely have trouble with your sleep quality or quantity, multiple nights a week.
Working with a sleep specialist or other another health care professional is important for managing insomnia because you can identify the root causes of your sleeplessness and establish a personalized treatment plan that addresses your specific needs.
“Modern sleep medicine has reached a point where most sleep disorder will improve when addressed correctly,” Pelayo says. “So you shouldn’t suffer with a sleep disorder anymore.”


























































































More on Sleep
How to Create a Sleep Sanctuary and Other Tips for a Good Night's Sleep
13 habits to give your body the rest it needs
6 Simple Strategies for Sleeping Through the Night
Tips for getting the deep sleep you need. Plus, how to get back to sleep if you wake in the wee hours
Sleep and Brain Health
Sleep habits and understanding the relationship between sleep and brain health are examined in this study of 40-plus adults
Wake Up More Refreshed With Our Smart Guide to Sleep
43 tips to help you fight those restless, endless nights and get the slumber you need
Recommended for You