AARP Hearing Center


Although roughly one-third of all adults don’t get as much sleep as they should, women seem to suffer disproportionately from not getting enough zzz’s.
A new study in Diabetes Care finds chronic insufficient sleep — even getting about six hours of sleep instead of the seven to nine recommended — increases insulin resistance, raising risk for diabetes in otherwise healthy women. This adds to past research that finds women are more likely than men to not get the recommended amount of shuteye, increasing their risk for everything from heart disease to depression.
To make matters worse, sleep deprivation and the negative health effects from it can be even more pronounced for women who’ve gone through menopause, researchers found in the Diabetes Care study and previous research published in the journal Hypertension. That study found that pushing back bedtime by an hour and a half, while waking up at the same time, led to an increase in blood pressure. Again, the effect was more pronounced for those who had gone through menopause.
In general, irrespective of age and other factors, “women tend to report poorer sleep quality overall,” says Marie-Pierre St-Onge, director of the Center of Excellence for Sleep & Circadian Research in the Columbia Irving Medical Center. St-Onge, who was a coauthor on the Diabetes Care and Hypertension studies, explains that hormonal changes, like those women experience during menopause, can further disrupt sleep. But that’s only one piece of a complex puzzle. Experts still don’t know all the answers for why women have a more fitful relationship with sleep than men – who, to be sure, also have significant issues getting the rest they need. One thing is certain: Sleep quality declines with age for both sexes.
Understanding women’s sleep struggles
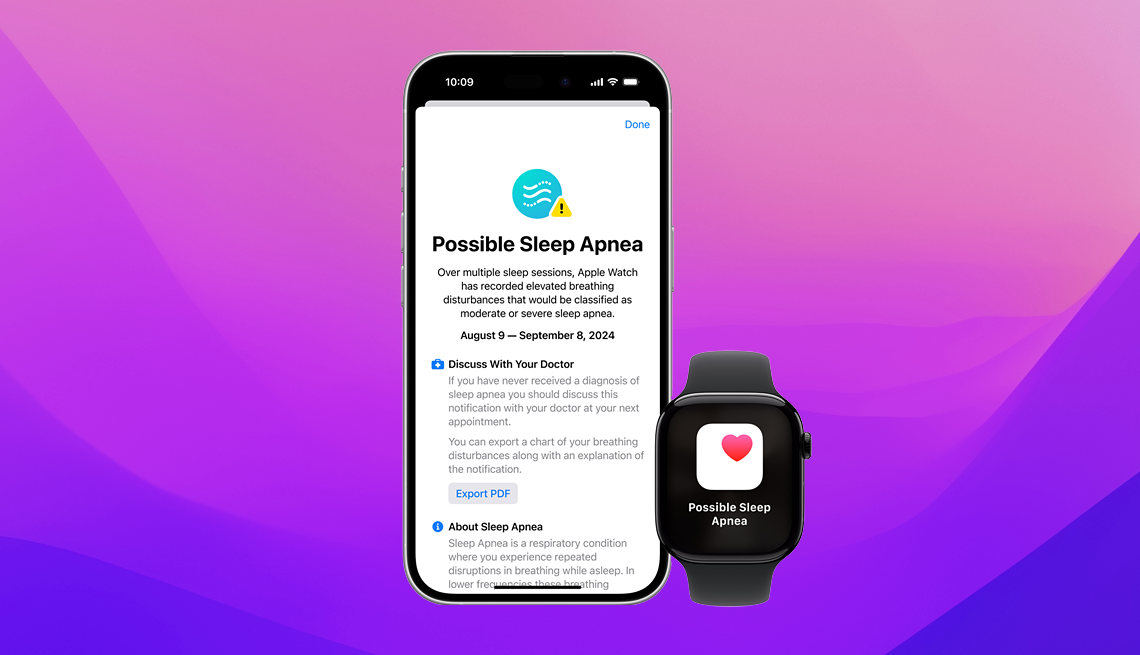
Getting to the root of your unrested development, or an emerging sleep problem, isn’t so easy. But experts say understanding, at least in part, what’s contributing to sleep loss is critical to adequately address the problem before it gets worse and torpedoes your health.
“Whenever we don’t sleep well, it literally makes every other component of our life and health worse,” says Marjorie Soltis, M.D., a neurologist and sleep medicine specialist at Duke Health in Durham, North Carolina. “It makes pain worse, it makes anxiety worse, it makes depression worse,” she says, to name a few examples.
Soltis adds that sleep deprivation causes medical conditions to progress more rapidly as well. The Centers for Disease Control and Prevention (CDC) notes that insufficient sleep contributes to or worsens mental health issues, brain disorders and chronic diseases.
Research finds women are more likely to experience insomnia, and the CDC reports that 17 percent of women have trouble falling asleep most nights, if not every night (when surveyed about the last 30 days), compared with almost 12 percent of men.
“There are so many different reasons, I think, why women tend to be more sleep-deprived than men,” Soltis says. “A lot of that can relate directly to the hormones that are involved in making us female, allowing us to have children – and, of course, having children and caring for children also definitely impacts the degree of sleep deprivation that women experience.” Frequently, sleep loss continues into later life as well, Soltis says, as women continue to take on a disproportionate share of family caregiving.
Women are also slightly more likely to be diagnosed with depression or anxiety, which can contribute to insomnia and insufficient sleep, she adds. Women commonly experience sleep problems during perimenopause and menopause when hormone levels become irregular and symptoms such as hot flashes, which tend to be worse at night, and night sweats make it especially difficult to get a good night’s rest.
The relationship between sleep and mental health is complex, and the effect of one on the other goes both ways, complicating diagnosis. So in the space of a quick visit with a primary care doctor, sleep-related problems can easily be overlooked. More pointedly, when “women seek care for various conditions, it may be written off as anxiety or depression when it may not actually be the case,” Soltis says. In cases where those issues are actually present, an underlying sleep problem that’s contributing could also be missed.
Getting to the root cause of restless nights
The first step to getting a better night’s rest involves taking sleep concerns seriously. As common as short sleep might be, experts say women and men often don’t think of it as a health issue at all.

















































































More From AARP
Medical Breakthroughs in Women’s Health
Advancements include new scans for dense breast tissue, help for hot flashes and more
6 Simple Strategies for Sleeping Through the Night
Tips for getting the deep sleep you need. Plus, how to get back to sleep if you wake in the wee hours
What to Do When Insomnia Makes You Afraid of Sleep
Is anxiety about sleeping keeping you awake at night? Here are 5 expert tips to reduce the stress
Recommended for You