AARP Hearing Center


Larry Goodman checks his weight, blood pressure and pulse every morning. Then, as he makes breakfast in his kitchen in Middletown, Delaware, a digital health company 3,000 miles away in California reviews his numbers.
“When you have a bad heart, every time you feel something you think, This is it,” says Goodman, 69. “But I don’t panic anymore. If there are numbers I don’t like, I get a call from my doctor’s office in 10 to 15 minutes.”
Like half of the 6.7 million Americans with heart failure, Goodman has a type called heart failure with reduced ejection fraction, meaning that the left side of his heart is too weak to pump enough blood out to his body.
Goodman first landed in the hospital with heart failure 15 years ago, unable to breathe and with fluid accumulating in his body, and for many years was in and out of the hospital.
Recognize early heart failure signs
Nearly 1 million U.S. adults are diagnosed each year with heart failure, but more than one-third of cases are missed by primary care physicians at early, more treatable stages, according to a 2021 study.
Don’t overlook the early warnings of heart failure:
- Shortness of breath
- A dry cough that’s worse at night
- Tiredness
- Nausea
- Low appetite
Leg swelling and an increase in the girth of your torso are potential indicators of fluid buildup when the heart isn’t pumping strongly, says Sourin Banerji, M.D. If you are diagnosed, make an appointment with a heart failure specialist, Banerji suggests.
A few years ago, he joined a program at ChristianaCare, a Delaware-based health system that offered a new digital monitoring program aimed at helping Black Americans with advanced heart failure get access to a breakthrough treatment: a combination of four drugs that together can save lives.
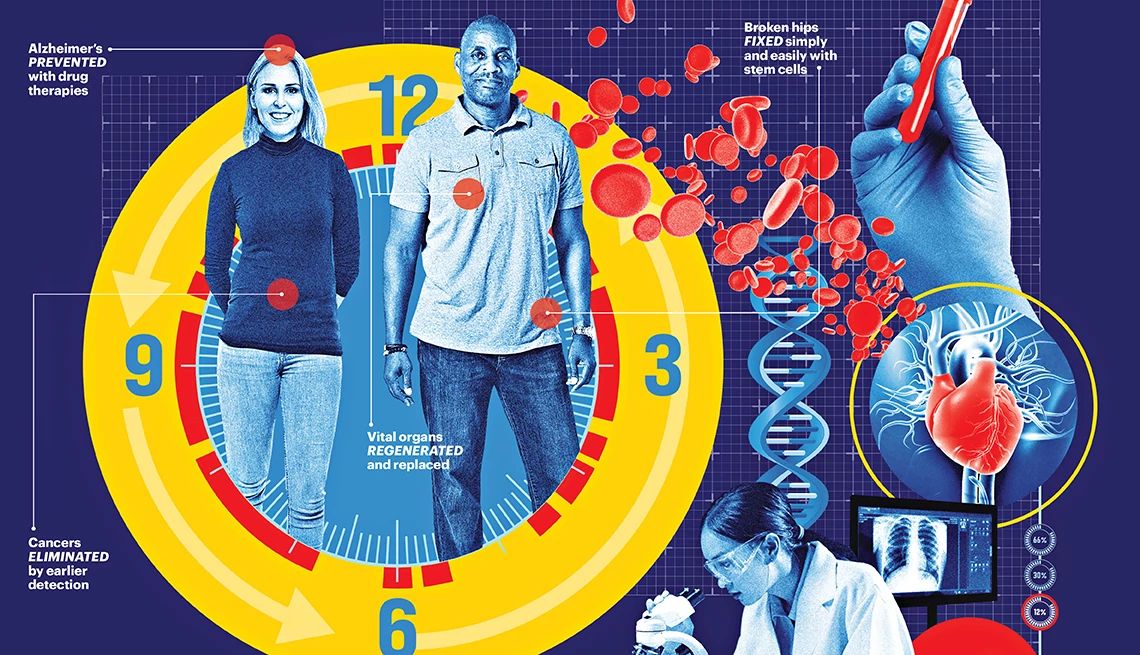
The drugs cut the risk of early death by 70 percent, improve symptoms and even help the heart function better. Without them, 10 to 15 percent of people with advanced heart failure are likely to die in just two years. In 2022, the American Heart Association and American College of Cardiology updated their guideline-directed medical therapy and for the first time recommended these four drugs, hailed as the “fantastic four.”
Yet most people who could benefit aren’t getting them. In a 2024 Duke University study of 33,036 older adults hospitalized for heart failure, 4 out of 5 were candidates for the drug combo but fewer than 1 in 6 got them. Among older adults, rates are especially low.
A big reason: It's not a one-size-fits-all therapy. Check-ins and follow-up are required to make sure each patient is getting the right dose of the medications for their unique needs, and that they’re able to tolerate any side effects.
But a tidal wave of new digital and remote monitoring programs is helping to change the trends. Instead of making frequent trips to the doctor or worrying about the drugs’ effects, those with heart failure can now track key health indicators at home with close monitoring by health care practitioners.
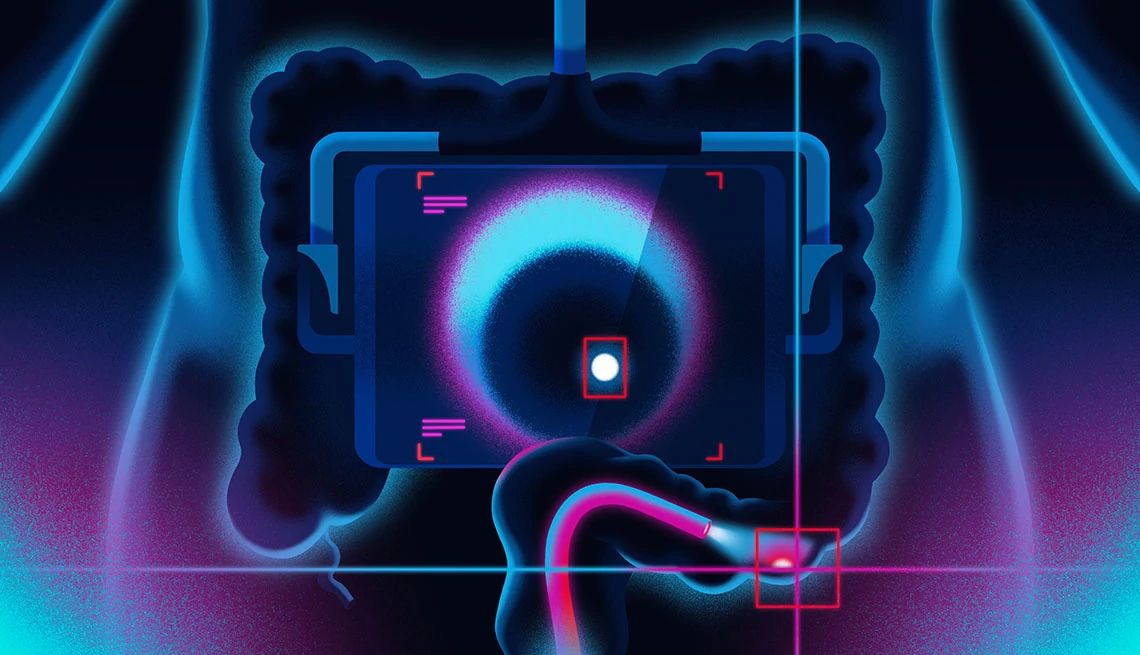
“It’s almost like the clinic is brought to the patients,” says Sourin Banerji, M.D., medical director of advanced heart failure at ChristianaCare Health. Other health systems are using a variety of home monitoring options, including an implanted sensor called CardioMEMS, approved by the U.S. Food and Drug Administration in 2022.



































































You Might Also Like
8 Ways to Get Heart Healthy
American Heart Association checklist now includes key components of cardiovascular health, from diet to sleep habits
11 Superfoods for Heart Health
Eat these to lower blood pressure, fight inflammation and slash heart disease and stroke riskTry These Tips for Living a Healthier Life
Small changes can add up to big mental and physical results
Recommended for You