AARP Hearing Center


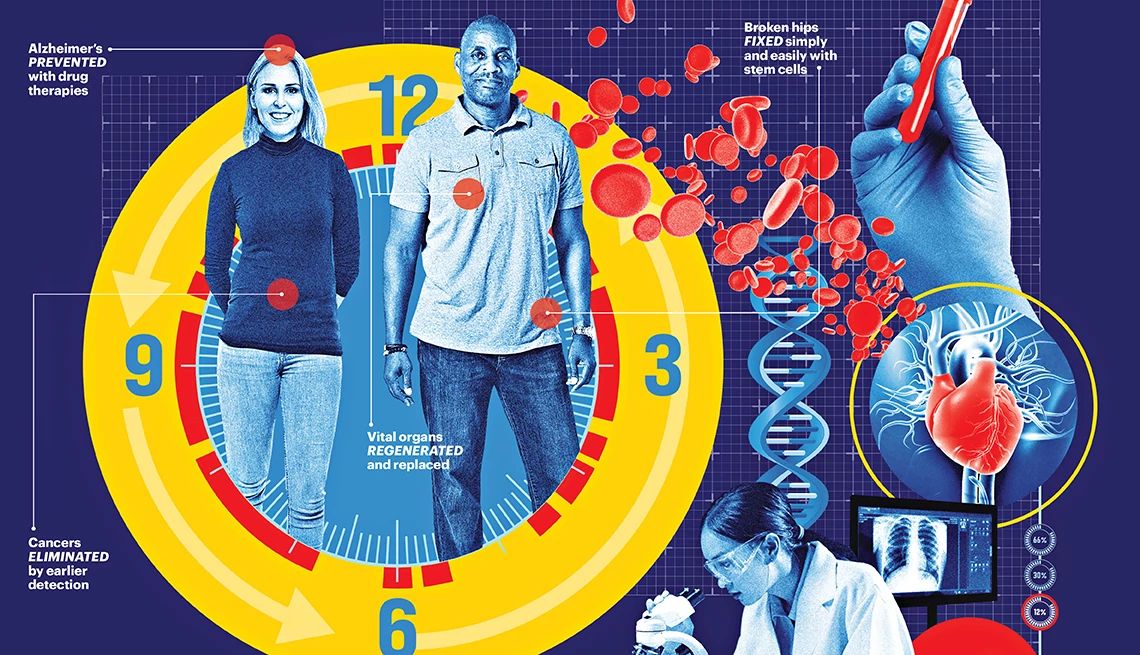
Research continues to revolutionize the way doctors and patients diagnose and treat a range of health conditions. Here’s a look at some of the latest medical advances and how they could help improve the lives of adults 50-plus.
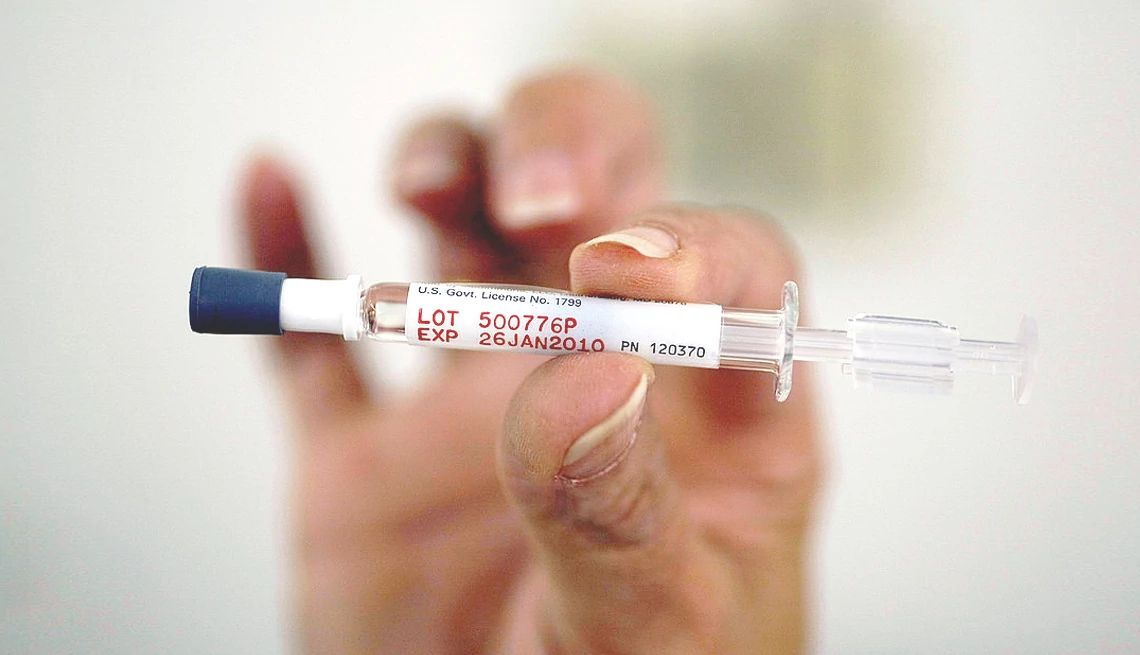
1. An at-home test for COVID and flu
Just in time for respiratory illness season, the U.S. Food and Drug Administration (FDA) has authorized an over-the-counter rapid test that can detect both COVID-19 and the flu — two common illnesses caused by different viruses that share a list of overlapping symptoms.
The test, from Healgen Scientific LLC, can detect proteins from the viruses that cause flu (influenza A and B) and COVID in about 15 minutes with a nose swab. It’s the first non-prescription combo test to hit the market with the FDA’s traditional approval process and not with emergency use authorization, like others available.
“The runny nose, the cough, the fever, the aches — that could be COVID, it could be influenza, it could be several other things, and being able to know what it is makes a huge difference, especially for people who are at higher risk for more severe illness,” says Gregory Martin, M.D., a professor of medicine at Emory University School of Medicine.
That’s because there are antiviral medications, like Paxlovid and Tamiflu, that can help keep an influenza or coronavirus infection from turning severe in high-risk individuals. But these treatments don’t work interchangeably, and they are most effective when started right away.
“Putting this in the hands of consumers allows people to figure out much more quickly and easily what's causing their symptoms,” Martin says. “And that makes a big difference for figuring out what to do next and what the treatment might be.”
According to the Centers for Disease Control and Prevention (CDC), symptoms for flu and COVID-19 can include:
- Fever or feeling feverish/having chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Sore throat
- Runny or stuffy nose
- Muscle pain or body aches
- Headache
- Vomiting
- Diarrhea
- Change in or loss of taste or smell
Another common bug known as RSV (short for respiratory syncytial virus) can also cause many of these symptoms. Martin says an at-home test that can distinguish between the three illnesses — COVID, flu and RSV — could be here as soon as next year. “It's getting easier and easier to be able to do multiple combination tests like that,” he says.
In an October news release, Healgen said it is scaling up its production to meet consumer demand for its flu/COVID test. The company told AARP that the test should be availble for purchase by the end of Novemeber on Amazon. At-home tests typically cost between $25 and $30 for a pack of two.



































































More From AARP
15 Things to Know About the Two New Alzheimer’s Drugs
These drugs are so new, many doctors aren’t prepared with answers to patients’ questionsA Combo COVID-Flu Vaccine Could Be Here Soon
A single shot could boost immune response and vaccination ratesWhat It’s Like to Catch COVID Over and Over
He’s had four bouts so far, and he says it has changed himRecommended for You