AARP Hearing Center

Four years ago, Rebecca Chopp, Ph.D., now 72, from Broomfield, Colorado, was living a packed life as a wife, mother, minister, theologian and chancellor at the University of Denver. At a routine annual checkup, she mentioned small changes to her doctor: Always a poor sleeper, she was now sleeping long hours; her social schedule for the university was rigorous, but lately she’d begun to feel less excited about being in large crowds; and she had recently gotten lost on the way to an appointment. Chopp had written it off to stress and her busy life, but that all changed when her doctor recommended a cognitive impairment exam, which led to an Alzheimer’s diagnosis.
At first, the news felt like a death sentence, sending Chopp and her husband, Fred Thibodeau, 76, reeling. Dementia ran in Chopp’s family. Growing up on a Kansas farm, she vividly recalled both her grandmother and mother at the end of their lives struggling with the devastating effects of Alzheimer’s. The neurologist that the couple met with told Chopp she wouldn’t be able to feed or dress herself in three years.
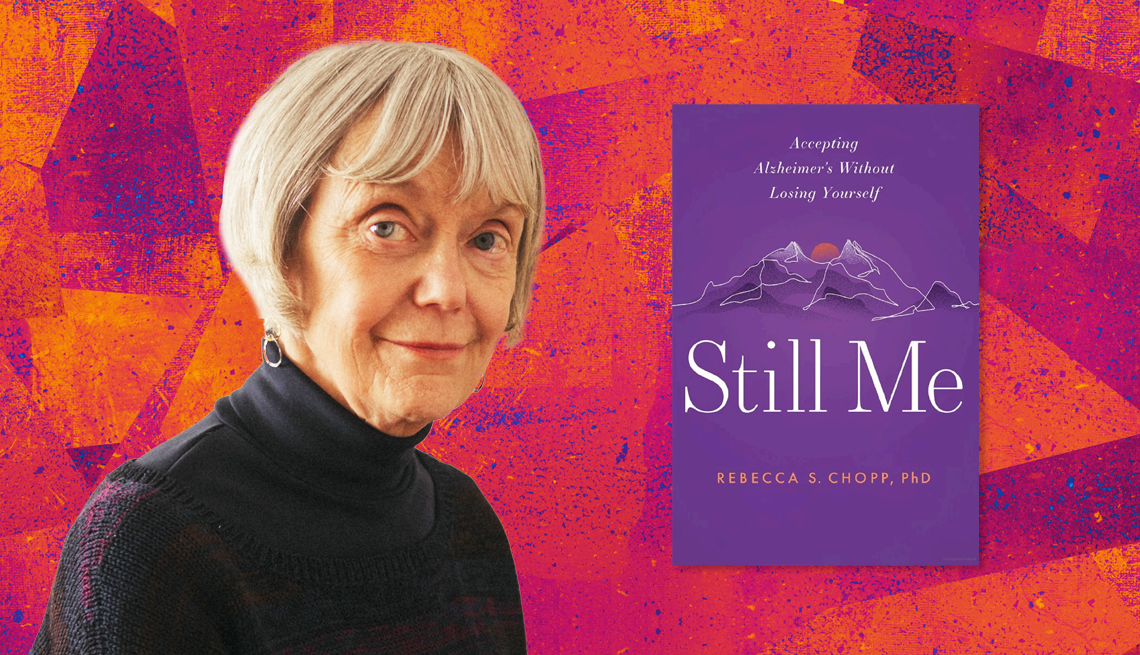
“We got home from that diagnosis, and Fred and I cried and cried. I’ve always done things for myself, and the thought of losing my independence was terrifying,” writes Chopp in her book Still Me – Accepting Alzheimer’s Without Losing Yourself. The book is a memoir, combined with research, science and a template for how to live with this disease, while trying to keep it from advancing. Her main message: “All of us need to refuse to surrender until we must.”
Chopp dug into the Alzheimer’s diagnosis with the rigor of an academic. There is new evidence, including a report in the journal Alzheimer’s Research &Therapy, that shows intensive lifestyle changes including diet, exercise and stress reduction may reduce the symptoms of mild cognitive impairment and early Alzheimer’s disease. Chopp was determined that the book could allow patients and caregivers to find hope, live with joy and fight back against this chronic disease, despite the knowledge that they will eventually lose everything.
Live long, better
When Chopp and Thibodeau sought a second opinion, they heard the same cold pronouncements of what Chopp “wouldn’t” be able to do. But it was the third neurologist, with the right bedside manner and healthy dose of empathy, who helped them both keep the door open for hope. The doctor advised the couple, to “live with joy,” and set them on a course to learn everything they could about how to help slow the advance of this insidious disease, which impacts more than 6.7 million Americans and an estimated 11 million unpaid caregivers.
“The more I learned about Alzheimer’s disease, the more I found I could experience joy and fight hard to stay well,” writes Chopp. From that point on, she was determined to do everything in her power to “stay me.” “Knowledge is power, and this disease, when diagnosed early, can develop slowly.”
Almost every researcher, neurologist and neuropsychologist told Chopp that if she could reduce the stress in her life, she would (most likely) live better and longer. Ann-Charlotte Granholm-Bentley, 65, a professor in the Department of Neurosurgery at University of Colorado and the former Director of the Knoebel Institute for Healthy Aging at the University of Denver was one of the first people Chopp sought out.
“Don’t panic,” advises Granholm-Bentley. “Take a measure of what you want in your life, live with the information for a while and don’t feel you have to make decisions right away.” She also stresses the importance of having a good physician. “If you aren’t happy with the way your neurologist talks to you, find one who has a better bedside manner.”
Make lifestyle changes
“When someone gets an Alzheimer’s diagnosis, I recommend they write a list of things they think they can change and the things they can’t or aren’t willing to change,” says Granholm-Bentley. “These will be changes affecting their work situation, diet and social network. There is a lot you can do.”


































































More From AARP
Help! My Doctor Won’t Listen to Me
Adam Rosenbluth, M.D., gives advice for getting your physician to really pay attention to you
How Family Caregivers Can Find Joy Through Understanding Dementia
Learning more about the disease can open up new avenues for happiness, connection