AARP Hearing Center

Whatever the fight was about, the origin was irrelevant; a ridiculous stand-off between two people who have been together long enough to know better. I was supposed to be cooking us dinner, followed by Netflix on the couch with a cuddle. Instead, I was lying in bed, vibrating like a tuning fork, heart beating as if I stood on a ledge, ready to jump.
Somehow, a conversation around the contents of a garden shed had taken a hairpin turn. He’d stormed off, changed course, and decided to drive south instead of waiting for the morning. And now I was alone, replaying the tape in my head, trying to disentangle what had happened.
And then it started. My chin began trembling uncontrollably, a wobbly tic of nerves and muscle, stopping and then starting again. My lips were numb. Was this the beginning of Parkinson’s, or some other dreaded neurological disease? I was bone-tired, scared and exhausted, yet flooded with adrenaline that made sleep impossible. No amount of counting backward or tapping on my arm was working. I stayed switched on high alert, attuned to danger through some ancestral hard-wired impulse.
Trauma memory
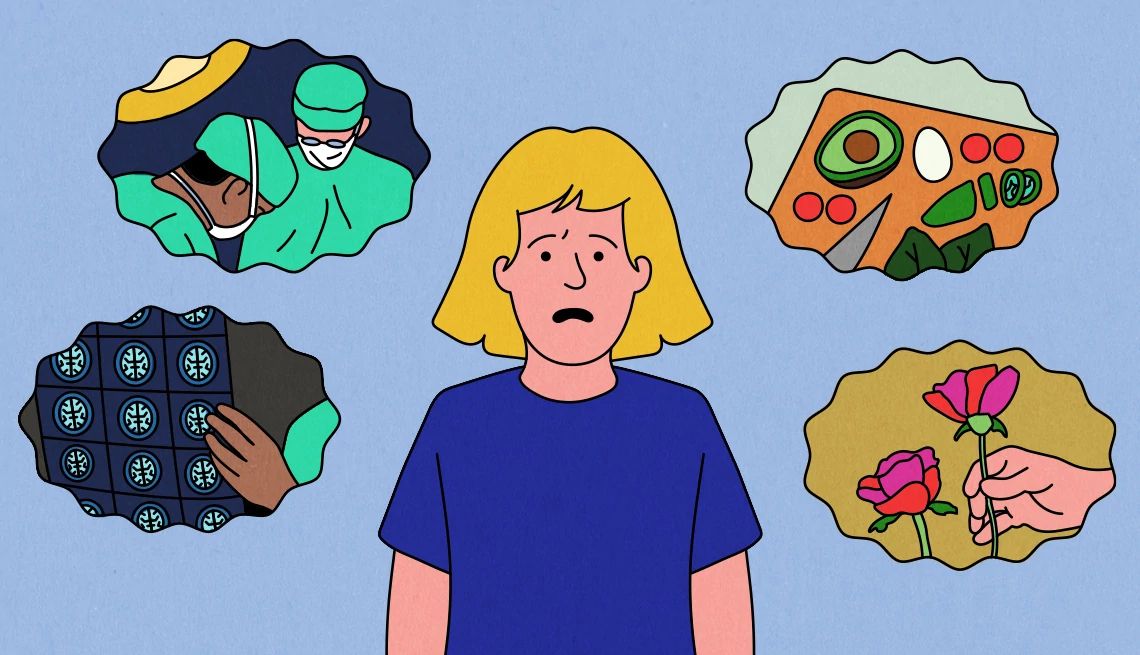
Navigating enduring relationships is a skill, but after trauma, life changes; the internal scar tissue has a long memory. And those scars aren’t topics most caregivers readily discuss.
I’d experienced this sense of extreme anxiety once before, months after my husband suffered a traumatic brain injury in Iraq in 2006. He was out of the danger zone between life and death, slowly improving, but still very much recovering in the rehabilitation hospital. Out of nowhere, I’d woken in the middle of the night, black thoughts and fears flying at me like crows, flooding me with panic. How would I take care of everyone? Would we need to sell the house if he couldn’t work? Questions and doubts swirled in my brain, as my body rose to the fear with a physical response, shivering, heart hammering, all of it overwhelming me.
The timing of that first experience made no sense, and yet it did. From the moment I’d gotten the phone call that Bob was injured by a roadside bomb in Iraq, I’d gone into a mental state I referred to as “The General” a toughness required to deal with the logistics, medical decisions and my four children’s needs. I blunted my emotions to cut through the endless tasks required to get through the day, as everything in those weeks felt like life and death. At times, it actually was.
































































More From AARP
How Worried Caregivers Can Avoid Becoming Anxious
Strategies to observe and stop harmful behavior in its tracksMore Than 60% Say Caregiving Increased Their Level of Stress, AARP Report Finds
Survey sheds light on daily stressors and shares how some manage anxiety, pressureYears After My Husband’s Injury in Iraq, I Still Have Caregiver PTSD
Traumatic events can have a long-term impact on a person’s ‘physical, emotional, social or spiritual well-being’
Recommended for You